Журнал «Медицина неотложных состояний» Том 19, №4, 2023
Вернуться к номеру
Періопераційна тромбоцитопенія: огляд сучасних рекомендацій та імплементація в клінічну практику
Авторы: Площенко Ю.О. (1), Новіков С.П. (2), Гавриш К.В. (2), Кущ В.М. (2), Карась Р.К. (2)
(1) — Дніпровський державний медичний університет, м. Дніпро, Україна
(2) — КНП «Міська клінічна лікарня № 4» ДМР, м. Дніпро, Україна
Рубрики: Медицина неотложных состояний
Разделы: Справочник специалиста
Версия для печати
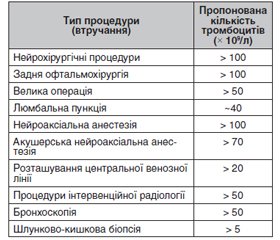
Тромбоцитопенія — це гетерогенна група розладів, визначальною ознакою яких є кількість тромбоцитів нижче від нижньої межі норми в 150 × 109/л, а виявлення цього розладу під час госпіталізації є достатньо поширеним феноменом. Тромбоцитопенія часто спостерігається у хворих різного профілю: у кардіологічних, акушерсько-гінекологічних, онкологічних, неврологічних і загальнотерапевтичних відділеннях, може перебігати і як самостійне захворювання, і як окремий симптом різних захворювань, що впливають на систему згортання крові. Етіологія тромбоцитопенії при критичному захворюванні часто є складною і багатофакторною. Тромбоцитопенія та можлива кровотеча становлять значні ризики для лікаря-анестезіолога в періопераційному періоді, що впливає на необхідність особливої уваги до пацієнта під час передопераційної підготовки, вибору оптимального методу знеболювання з урахуванням усіх факторів і якісної післяопераційної інтенсивної терапії. У нашій статті ми розглянули сучасні стратегії ведення пацієнтів з періопераційною тромбоцитопенією, запропоновані для досягнення безпечного позитивного результату лікування, і на прикладі двох клінічних випадків показали можливість успішного використання таких стратегій, як призначення стероїдів, антифібринолітичних засобів, уведення внутрішньовенного глобуліну, застосування агоністів рецепторів тромбопоетину і оптимізація гематокриту в умовах сумісної роботи мультидисциплінарної команди — анестезіологів, хірургів і гематологів. Для поліпшення результатів лікування хворих з тромбоцитопеніями і максимального зниження ризиків пацієнтів у періопераційному періоді ми рекомендуємо мультидисциплінарний підхід у підготовці й веденні таких хворих та індивідуальне застосування різних періопераційних стратегій для збільшення кількості тромбоцитів і зменшення інтраопераційної кровотечі у хворих з тромбоцитопеніями різної етіології.
Thrombocytopenia is a heterogeneous group of disorders characterized by a platelet count below the lower limit of normal (150 × 109/L), and detection of this disorder during hospitalization is a fairly common phenomenon. Thrombocytopenia is often observed in patients of various profiles: in cardiology, obstetrics and gynecology, cancer, neurology and general therapeutic departments and can occur as an independent condition or as a separate symptom of various diseases affecting the blood coagulation system. The etiology of thrombocytopenia in critical illness is often complex and multifactorial. Thrombocytopenia and possible bleeding represent significant risks for the anesthesiologist in the perioperative period, which affects the need for special attention to a patient during preoperative preparation, choosing the optimal method of anasthesia taking into account all factors, and high-quality postoperative intensive care. In our article, we reviewed the current proposed approaches to perioperative thrombocytopenia to achieve a safe positive treatment outcome and, using the example of two clinical cases, showed the possibility of successful use of strategies such as administration of steroids, antifibrinolytic agents, intravenous globulin, thrombo-poietin receptor agonists, and hematocrit optimization in conditions of the joint work of a multidisciplinary team — anesthesiologists, surgeons and hematologists. To improve the results of treatment for thrombocytopenia and to minimize the risks in the perioperative period, we recommend a multidisciplinary approach to the preparation and management of such patients and the individual use of various perioperative strategies to increase the number of platelets and reduce intraoperative bleeding in case of thrombocytopenia of various etiologies.
тромбоцитопенія; періопераційний період; інтенсивна терапія
thrombocytopenia; perioperative period; intensive care
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Glance L.G., Blumberg N., Eaton M.P. et al. Preoperative thrombocytopenia and postoperative outcomes after noncardiac surgery. Anesthesiology. 2014. Vol. 120. P. 62-75. doi: 10.1097/ALN.0b013e3182a4441f.
- Malpani R., Bovonratwet P., Clark M.G. et al. Preoperative high, as well as low, platelet counts correlate with adverse outcomes after elective total hip arthroplasty. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2020. Vol. 4. P. e2000049. doi: 10.5435/JAAOSGlobal-D-20-00049.
- Malpani R., Haynes M.S., Clark M.G. et al. Abnormally high, as well as low, preoperative platelet counts correlate with adverse outcomes and readmissions after elective total knee arthroplasty. J. Arthroplasty. 2019. Vol. 34. P. 1670-1676. doi: 10.1016/j.arth.2019.04.012.
- Weil I.A., Kumar P., Seicean S. et al. Platelet count abnormalities and perioperative outcomes in adults undergoing elective, noncardiac surgery. PLoS One. 2019. Vol. 14. P. e0212191. doi: 10.1371/journal.pone.0212191.
- Kertai M.D., Zhou S., Karhausen J.A. et al. Platelet counts, acute kidney injury, and mortality after coronary artery bypass grafting surgery. Anesthesiology. 2016. Vol. 124. P. 339-352. doi: 10.1097/ALN.0000000000000959.
- Thachil J., Warkentin T.E. How do we approach thrombocytopenia in critically ill patients? Br. J. Haematol. 2017. Vol. 177. P. 27-38. doi: 10.1111/bjh.14482.
- Dewitte A., Lepreux S., Villeneuve J. et al. Blood platelets and sepsis pathophysiology: a new therapeutic prospect in critically ill patients? Ann. Intensive Care. 2017. Vol. 7. P. 115. doi: 10.1186/s13613-017-0337-7.
- Rahi M.S., Jindal V., Reyes S.P. et al. Hematologic disorders associated with COVID-19: a review. Ann. Hematol. 2021. Vol. 100. P. 309-320. doi: 10.1007/s00277-020-04366-y.
- Afdhal N., McHutchison J., Brown R. et al. Thrombocytopenia associated with chronic liver disease. J. Hepatol. 2008. Vol. 48. P. 1000-1007. doi: 10.1016/j.jhep.2008.03.009.
- Stasi R. How to approach thrombocytopenia. Hematology Am. Soc. Hematol. Educ. Program. 2012. Vol. 2012. P. 191-197. doi: 10.1182/asheducation-2012.1.191.
- Reese J.A., Peck J.D., Deschamps D.R. et al. Platelet counts during pregnancy. N. Engl. J. Med. 2018. Vol. 379. P. 32-43. doi: 10.1056/NEJMoa1802897.
- van den Akker E.S., Oepkes D. Fetal and neonatal alloimmune thrombocytopenia. Best Pract. Res. Clin. Obstet Gynaecol. 2008. Vol. 22. P. 3-14. doi: 10.1016/j.bpobgyn.2007.08.001.
- Aster R.H., Curtis B.R., McFarland J.G. et al. Drug-induced immune thrombo- cytopenia: pathogenesis, diagnosis, and management. J. Thromb. Haemost. 2009. Vol. 7. P. 911-918. doi: 10.1111/j.1538-7836.2009.03360.x.
- Nagrebetsky A., Al-Samkari H., Davis N.M. et al. Perioperative thrombocytopenia: evidence, evaluation, and emerging therapies. Br. J. Anaesth. 2019. Vol. 122. P. 19-31. doi: 10.1016/j.bja.2018.09.010.
- Arepally G.M. Heparin-induced thrombocytopenia. Blood. 2017. Vol. 129. P. 2864-2872. doi: 10.1182/blood-2016-11-709873.
- Bobba R.K., Doll D.C. Platelet satellitism as a cause of spurious thrombocytopenia. Blood. 2012. Vol. 119. P. 4100. doi: 10.1182/blood-2011-08-369173.
- Lo G.K., Juhl D., Warkentin T.E., Sigouin C.S. et al. Evaluation of pretest clinical score (4 T’s) for the diagnosis of heparin-induced thrombocytopenia in two clinical settings. J. Thromb. Haemost. 2006. Vol. 4. P. 759-765. doi: 10.1111/j.1538-7836.2006.01787.x.
- Warkentin T.E., Smythe M.A., Ali M.A. et al. Serotonin-release assay-positive but platelet factor 4-dependent enzyme-immunoassay negative: HIT or not HIT? Am. J. Hematol. 2021. Vol. 96. P. 320-329. doi: 10.1002/ajh.26075.
- Piel-Julian M.L., Mahévas M., Germain J. et al. Risk factors for bleeding, including platelet count threshold, in newly diagnosed immune thrombocytopenia adults. J. Thromb. Haemost. 2018. Vol. 16. P. 1830-1842. doi: 10.1111/jth.14227.
- Orsini S., Noris P., Bury L. et al. Bleeding risk of surgery and its prevention in patients with inherited platelet disorders. Haematologica. 2017. Vol. 102. P. 1192-1203. doi: 10.3324/haematol.2016.160754.
- Thiele T., Greinacher A. Platelet transfusion in perioperative medicine. Semin. Thromb. Hemost. 2020. Vol. 46. P. 50-61. doi: 10.1055/s-0039-1697951.
- Estcourt L.J., Birchall J., Allard S. et al. Guidelines for the use of platelet transfusions. Br. J. Haematol. 2017. Vol. 176. P. 365-394. doi: 10.1111/bjh.14423.
- Kaufman R.M., Djulbegovic B., Gernsheimer T. et al. Platelet transfusion: a clinical practice guideline from the AABB. Ann. Intern. Med. 2015. Vol. 162. P. 205-213. doi: 10.7326/M14-1589.
- Vavricka S.R., Walter R.B., Irani S. et al. Safety of lumbar puncture for adults with acute leukemia and restrictive prophylactic platelet transfusion. Ann. Hematol. 2003. Vol. 82. P. 570-573. doi: 10.1007/s00277-003-0707-0.
- van Veen J.J., Nokes T.J., Makris M. The risk of spinal haematoma following neuraxial anaesthesia or lumbar puncture in thrombocytopenic individuals. Br. J. Haematol. 2010. Vol. 148. P. 15-25. doi: 10.1111/j.1365-2141.2009.07899.x.
- Zeidler K., Arn K., Senn O. et al. Optimal preprocedural platelet transfusion threshold for central venous catheter insertions in patients with thrombocytopenia. Transfusion. 2011. Vol. 51. P. 2269-2276. doi: 10.1111/j.1537-2995.2011.03147.x.
- Warner M.A., Woodrum D., Hanson A. et al. Preprocedural platelet transfusion for patients with thrombocytopenia undergoing interventional radiology procedures is not associated with reduced bleeding complications. Transfusion. 2017. Vol. 57. P. 890-898. doi: 10.1111/trf.13996.
- Nandagopal L., Veeraputhiran M., Jain T. et al. Broncho-scopy can be done safely in patients with thrombocytopenia. Transfusion. 2016. Vol. 56. P. 344-348. doi: 10.1111/trf.13348.
- Bernstein J., Hua B., Kahana M. et al. Neuraxial anesthesia in parturients with low platelet counts. Anesth. Analg. 2016. Vol. 123. P. 165-167. doi: 10.1213/ANE.0000000000001312.
- Lee L.O., Bateman B.T., Kheterpal S. et al. Risk of epidural hematoma after neuraxial techniques in thrombocytopenic parturients: a report from the multicenter perioperative outcomes group. Anesthesiology. 2017. Vol. 126. P. 1053-1063. doi: 10.1097/ALN.0000000000001630.
- Levy N., Goren O., Cattan A. et al. Neuraxial block for delivery among women with low platelet counts: a retrospective analysis. Int. J. Obstet. Anesth. 2018. Vol. 35. P. 4-9. doi: 10.1016/j.ijoa.2018.01.006.
- Bauer M.E., Toledano R.D., Houle T. et al. Lumbar neuraxial procedures in thrombocytopenic patients across populations: a systematic review and meta-analysis. J. Clin. Anesth. 2020. Vol. 61. P. 109666. doi: 10.1016/j.jclinane.2019.109666.
- Estcourt L.J., Malouf R., Hopewell S. et al. Use of platelet transfusions prior to lumbar punctures or epidural anaesthesia for the prevention of complications in people with thrombocytopenia. Cochrane Database Syst. Rev. 2018. Vol. 4. Article No. CD011980. doi: 10.1002/14651858.CD011980.pub3.
- Bailey L.J., Shehata N., De France B. et al. Obstetric neuraxial anesthesia at low platelet counts in the context of immune thrombocytopenia: a systematic review and meta-analysis. Can. J. Anaesth. 2019. Vol. 66. P. 1396-1414. doi: 10.1007/s12630-019-01420-w.
- Ho A.M., Mizubuti G.B., Ho A.K. Safety of spinal anesthesia in thrombocytopenic patients: are there lessons to be learnt from oncology? Reg. Anesth. Pain Med. 2019. Vol. 44. P. 29-31. doi: 10.1136/rapm-2018-000011.
- Bauer M.E., Arendt K., Beilin Y. et al. The Society for Obstetric Anesthesia and Perinatology Interdisciplinary Consensus Statement on Neuraxial Procedures in Obstetric Patients With Thrombocytopenia. Anesth. Analg. 2021. Vol. 132(6). P. 1531-1544. doi: 10.1213/ANE.0000000000005355.
- Estcourt L.J., Malouf R., Doree C. et al. Prophylactic platelet transfusions prior to surgery for people with a low platelet count. Cochrane Database Syst. Rev. 2018. Vol. 9. Article No. CD012779. doi: 10.1002/14651858.CD012779.pub2.
- Levy J.H., Rossaint R., Zacharowski K. et al. What is the evidence for platelet transfusion in perioperative settings? Vox Sang. 2017. Vol. 112. P. 704-712. doi: 10.1111/vox.12576.
- Yanagawa B., Ribeiro R., Lee J. et al. Platelet transfusion in cardiac surgery: a systematic review and meta-analysis. Ann. Thorac. Surg. 2021. Vol. 111. P. 607-614. doi: 10.1016/j.athoracsur.2020.04.139.
- Goel R., Ness P.M., Takemoto C.M. et al. Platelet transfusions in platelet consumptive disorders are associated with arterial thrombosis and in-hospital mortality. Blood. 2015. Vol. 125. P. 1470-1476. doi: 10.1182/blood-2014-10-605493.
- Swisher K.K., Terrell D.R., Vesely S.K. et al. Clinical outcomes after platelet transfusions in patients with thrombotic thrombocytopenic purpura. Transfusion. 2009. Vol. 49. P. 873-887. doi: 10.1111/j.1537-2995.2008.02082.x.
- Hopkins C.K., Goldfinger D. Platelet transfusions in heparin-induced thrombocytopenia: a report of four cases and review of the literature. Transfusion. 2008. Vol. 48. P. 2128-2132. doi: 10.1111/j.1537-2995.2008.01822.x.
- Squizzato A., Hunt B.J., Kinasewitz G.T. et al. Supportive management strategies for disseminated intravascular coagulation. An international consensus. Thromb. Haemost. 2016. Vol. 115. P. 896-904. doi: 10.1160/TH15-09-0740.
- Belizaire R., Makar R.S. Non-alloimmune mechanisms of thrombocytopenia and refractoriness to platelet transfusion. Transfus. Med. Rev. 2020. Vol. 34. P. 242-249. doi: 10.1016/j.tmrv.2020.09.002.
- Saris A., Pavenski K. Human leukocyte antigen alloimmunization and alloimmune platelet refractoriness. Transfus. Med. Rev. 2020. Vol. 34. P. 250-257. doi: 10.1016/j.tmrv.2020.09.010.
- Nurden A.T. Acquired antibodies to alphaIIbbeta3 in glanzmann thrombasthenia: from transfusion and pregnancy to bone marrow transplants and beyond. Transfus. Med. Rev. 2018. Vol. 18. P. 30037-3. doi: 10.1016/j.tmrv.2018.05.002.
- Mithoowani S., Gregory-Miller K., Goy J. et al. High-dose dexamethasone compared with prednisone for previously untreated primary immune thrombocytopenia: a systematic review and meta-analysis. Lancet Haematol. 2016. Vol. 3. P. e489-e496. doi: 10.1016/S2352-3026(16)30109-0.
- Ammann E.M., Haskins C.B., Fillman K.M. et al. Intravenous immune globulin and thromboembolic adverse events: a systematic review and meta-analysis of RCTs. Am. J. Hematol. 2016. Vol. 91. P. 594-605. doi: 10.1002/ajh.24358.
- George J.N., Raskob G.E., Vesely S.K. et al. Initial management of immune thrombocytopenic purpura in adults: a randomized controlled trial comparing intermittent anti-D with routine care. Am. J. Hematol. 2003. Vol. 74. P. 161-169. doi: 10.1002/ajh.10424.
- Kuter D.J. The biology of thrombopoietin and thrombopoietin receptor agonists. Int. J. Hematol. 2013. Vol. 98. P. 10-23. doi: 10.1007/s12185-013-1382-0.
- Marshall A.L., Goodarzi K., Kuter D.J. Romiplostim in the management of the thrombocytopenic surgical patient. Transfusion. 2015. Vol. 55. P. 2505-2510. doi: 10.1111/trf.13181.
- Ramakrishna R., Rehman A., Ramakrishna S. et al. Use of romiplostim in patients with chronic idiopathic thrombocytopenic purpura during perioperative period. Intern. Med. J. 2015. Vol. 45. P. 718-724. doi: 10.1111/imj.12794.
- Al-Samkari H., Marshall A.L., Goodarzi K. et al. Romiplostim for the management of perioperative thrombocytopenia. Br. J. Haematol. 2018. Vol. 182. P. 106-113. doi: 10.1111/bjh.15280.
- Arnold D.M., Heddle N.M., Cook R.J. et al. Perioperative oral eltrombopag versus intravenous immunoglobulin in patients with immune thrombocytopenia: a noninferiority, multicentre, randomised trial. Lancet Haematol. 2020. Vol. 7. P. e640-e648. doi: 10.1016/S2352-3026(20)30227-1.
- Saab S., Brown R.S. Management of thrombocytopenia in patients with chronic liver disease. Dig. Dis. Sci. 2019. Vol. 64. P. 2757-2768. doi: 10.1007/s10620-019-05615-5.
- Michelson A.D., Smolensky Koganov E., Forde E.E. et al. Avatrombopag increases platelet count but not platelet activation in patients with thrombocytopenia resulting from liver disease. J. Thromb. Haemost. 2018. Vol. 16. P. 2515-2519. doi: 10.1111/jth.14295.
- Khemichian S., Terrault N.A. Thrombopoietin receptor agonists in patients with chronic liver disease. Semin. Thromb. Hemost. 2020. Vol. 46. P. 682-692. doi: 10.1055/s-0040-1715451.
- Saab S., Bernstein D., Hassanein T. et al. Treatment options for thrombocytopenia in patients with chronic liver disease undergoing a scheduled procedure. J. Clin. Gastroenterol. 2020. Vol. 54. P. 503-511. doi: 10.1097/MCG.0000000000001338.
- Lindquist I., Olson S.R., Li A. et al. The efficacy and safety of thrombopoietin receptor agonists in patients with chronic liver disease undergoing elective procedures: a systematic review and meta-analysis. Platelets. 2022. Vol. 33(1). P. 66-72. doi: 10.1080/09537104.2020.1859102.
- Vo P., Purev E., West K.A. et al. A pilot trial of complement inhibition using eculizumab to overcome platelet transfusion refractoriness in human leukocyte antigen alloimmunized patients. Br. J. Haematol. 2020. Vol. 189. P. 551-558. doi: 10.1111/bjh.16385.
- Scully M., Cataland S.R., Peyvandi F. et al. Caplacizumab treatment for acquired thrombotic thrombocytopenic purpura. N. Engl. J. Med. 2019. Vol. 380. P. 335-346. doi: 10.1056/NEJMoa1806311.
- Colucci G., Stutz M., Rochat S. et al. The effect of desmopressin on platelet function: a selective enhancement of procoagulant COAT platelets in patients with primary platelet function defects. Blood. 2014. Vol. 123. P. 1905-1916. doi: 10.1182/blood-2013-04-497123.
- Stockschlaeder M., Schneppenheim R., Budde U. Update on von Willebrand factor multimers: focus on high-molecular-weight multimers and their role in hemostasis. Blood Coagul. Fibrinolysis. 2014. Vol. 25. P. 206-216. doi: 10.1097/MBC.0000000000000065.
- Swieringa F., Lance M.D., Fuchs B. et al. Desmopressin treatment improves platelet function under flow in patients with postoperative bleeding. J. Thromb. Haemost. 2015. Vol. 13. P. 1503-1513. doi: 10.1111/jth.13007.
- Desborough M.J., Oakland K., Brierley C. et al. Desmopressin use for mini-mising perioperative blood transfusion. Cochrane Database Syst. Rev. 2017. Vol. 7. Article No. CD001884. doi: 10.1002/14651858.CD001884.pub3.
- Lim C.C., Siow B., Choo J.C.J. et al. Desmopressin for the prevention of bleeding in percutaneous kidney biopsy: efficacy and hyponatremia. Int. Urol. Nephrol. 2019. Vol. 51. P. 995-1004. doi: 10.1007/s11255-019-02155-9.
- Estcourt L.J., McQuilten Z., Powter G. et al. The TREATT Trial (TRial to EvaluAte Tranexamic acid therapy in Thrombocytopenia): safety and efficacy of tranexamic acid in patients with haematological malignancies with severe thrombocytopenia: study protocol for a double-blind randomised controlled trial. Trials. 2019. Vol. 20. P. 592. doi: 10.1186/s13063-019-3663-2.
- Jarvis G.E., Atkinson B.T., Frampton J. et al. Thrombin-induced conversion of fibrinogen to fibrin results in rapid platelet trapping which is not dependent on platelet activation or GPIb. Br. J. Pharmacol. 2003. Vol. 138. P. 574-583. doi: 10.1038/sj.bjp.0705095.
- Velik-Salchner C., Haas T., Innerhofer P. et al. The effect of fibrinogen concentrate on thrombocytopenia. J. Thromb. Haemost. 2007. Vol. 5. P. 1019-1025. doi: 10.1111/j.1538-7836.2007.02481.x.
- Xu M., Luo L., Du M. et al. Fibrinogen levels are associated with bleeding in patients with primary immune thrombocytopenia. Platelets. 2020. Vol. 31. P. 763-770. doi: 10.1080/09537104.2019.1678115.
- Ranucci M., Baryshnikova E., Ranucci M. et al.; Surgical and Clinical Outcome Research Groupe. Fibrinogen levels compensation of thrombocytopenia-induced bleeding following cardiac surgery. Int. J. Cardiol. 2017. Vol. 249. P. 96-100. doi: 10.1016/j.ijcard.2017.09.157.
- Kristensen J., Killander A., Hippe E. et al. Clinical experience with recombinant factor VIIa in patients with thrombocytopenia. Haemostasis. 1996. Vol. 26 (Suppl. 1). P. 159-164. doi: 10.1159/000217260.
- Brennan Y., Levade M., Ward C.M. Acquired platelet function disorders. Thromb Res. 2020. Vol. 196. P. 561-568. doi: 10.1016/j.thromres.2019.06.009.
- Chu T., Tang Y., Wang H. et al. Efficacy of recombinant factor VIIa for severe bleeding complicated by platelet transfusion refractoriness in patients with hematologic malignancies. Thromb. Res. 2017. Vol. 160. P. 14-18. doi: 10.1016/j.thromres.2017.10.015.
- Monroe D.M., Hoffman M., Roberts H.R. Platelets and thrombin generation. Arterioscler. Thromb. Vasc. Biol. 2002. Vol. 22. P. 1381-1389. doi: 10.1161/01.atv.0000031340.68494.34.
- Chowdary P., Hamid C., Slatter D. et al. Impaired platelet-dependent thrombin generation associated with thrombocytopenia is improved by prothrombin complex concentrates in vitro. Res. Pract. Thromb. Haemost. 2020. Vol. 4. P. 334-342. doi: 10.1002/rth2.12310.
- Uhl L., Assmann S.F., Hamza T.H. et al. Laboratory predictors of bleeding and the effect of platelet and RBC transfusions on bleeding outcomes in the PLADO trial. Blood. 2017. Vol. 130. P. 1247-1258. doi: 10.1182/blood-2017-01-757930.
- Valeri C.R., Cassidy G., Pivacek L.E. et al. Anemia-induced increase in the bleeding time: implications for treatment of nonsurgical blood loss. Transfusion. 2001. Vol. 41. P. 977-983. doi: 10.1046/j.1537-2995.2001.41080977.x.
- Spann A.P., Campbell J.E., Fitzgibbon S.R. et al. The effect of hematocrit on platelet adhesion: experiments and simulations. Biophys. J. 2016. Vol. 111. P. 577-588. doi: 10.1016/j.bpj.2016.06.024.
- Carson J.L., Guyatt G., Heddle N.M. et al. Clinical practice guidelines from the aabb: red blood cell transfusion thresholds and sto-rage. JAMA. 2016. Vol. 316. P. 2025-2035. doi: 10.1001/jama.2016.9185.