Международный эндокринологический журнал Том 17, №1, 2021
Вернуться к номеру
Модель прогнозування тяжкості діабетичної ретинопатії, отримана на основі ендотеліальної дисфункції та маркерів гіпоксії
Авторы: Ya.V. Sirman, I.V. Savytskyi, N.I. Preys
State Institution “Ukrainian Research Institute of Transport Medicine of the Ministry of Health of Ukraine”,
Odesa, Ukraine
Рубрики: Эндокринология
Разделы: Клинические исследования
Версия для печати
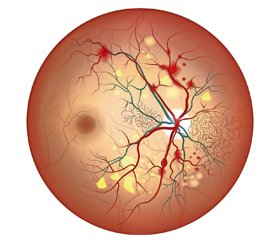
Актуальність. Діабетична ретинопатія — специфічне мікросудинне ускладнення цукрового діабету. Вона залишається провідною причиною втрати зору в працездатного дорослого населення. У пацієнтів із тяжким ступенем діабетичної ретинопатії спостерігається зниження якості життя та погіршення фізичного, емоційного й соціального благополуччя. До того ж на цю когорту пацієнтів витрачається більше ресурсів системи охорони здоров’я. Розробка математичних моделей прогнозування дозволяє більш різнобічно аналізувати експериментальні та клінічні дані. Мета дослідження: розробка моделі прогнозування тяжкості діабетичної ретинопатії на основі маркерів ендотеліальної дисфункції та гіпоксії. Матеріали та методи. Використовували стрептозотоцинову модель цукрового діабету 2-го типу. Визначали рівні фактора Віллебранда, ендотеліну-1, 2,3-дифосфогліцерату, що використовували як змінні. Перехід непроліферативної фази діабетичної ретинопатії в проліферативну на 180-ту добу експерименту підтверджували гістологічно. Результати. Розроблена математична модель для прогнозування досліджуваного патологічного стану на основі біохімічних аналізів крові на ранніх етапах експерименту. Доведена інформативність маркерів ендотеліальної дисфункції, фактора Віллебранда й ендотеліну-1, у прогнозуванні переходу непроліферативної діабетичної ретинопатії в проліферативну. Встановлено значущість визначення рівня 2,3-дифосфогліцерату в еритроцитах разом iз зазначеними вище маркерами функціонального статусу ендотелію на 30-ту добу для прогнозування подальшого перебігу хвороби. Висновки. Доведено значущість показника 2,3-дифосфогліцерату в еритроцитах і зазначених маркерів функціонального статусу ендотелію на 30-ту добу для прогнозування подальшого перебігу досліджуваного патологічного процесу.
Актуальность. Диабетическая ретинопатия — специфическое микрососудистое осложнение сахарного диабета. Она остается ведущей причиной потери зрения у трудоспособного взрослого населения. У пациентов с тяжелой степенью диабетической ретинопатии наблюдается снижение качества жизни и ухудшение физического, эмоционального и социального благополучия. К тому же на эту когорту пациентов затрачивается больше ресурсов системы здравоохранения. Разработка математических моделей прогнозирования позволяет более разносторонне анализировать экспериментальные и клинические данные. Цель исследования: разработка модели прогнозирования тяжести диабетической ретинопатии на основе маркеров эндотелиальной дисфункции и гипоксии. Материалы и методы. Использовали стрептозотоциновую модель сахарного диабета 2-го типа. Определяли уровни фактора Виллебранда, эндотелина-1, 2,3-дифосфоглицерата, которые использовали в качестве переменных. Переход непролиферативной фазы диабетической ретинопатии в пролиферативную на 180-е сутки эксперимента подтверждали гистологически. Результаты. Разработана математическая модель для прогнозирования исследуемого патологического состояния на основе биохимических анализов крови на ранних этапах эксперимента. Доказана информативность маркеров эндотелиальной дисфункции, фактора Виллебранда и эндотелина-1, в прогнозировании перехода непролиферативной диабетической ретинопатии в пролиферативную. Установлена значимость определения уровня 2,3-дифосфоглицерата в эритроцитах вместе с указанными выше маркерами функционального статуса эндотелия на 30-й день для прогнозирования дальнейшего течения болезни. Выводы. Доказана значимость показателя 2,3-дифосфоглицерата в эритроцитах и указанных маркеров функционального статуса эндотелия на 30-й день для прогнозирования дальнейшего течения исследуемого патологического процесса.
Background. According to a wide range of authors, eye damage caused by diabetes mellitus accounts for 80–90 % of the total number of disorders. The development of mathematical predictive models allows for a more versatile analysis of experimental and clinical data. The purpose of the study was to develop a model for predicting the severity of diabetic retinopathy based on a review of markers of endothelial dysfunction and hypoxia. Materials and methods. We used a streptozotocin model of type 2 diabetes mellitus. Determined von Willebrand factor, endothelin-1, 2,3-diphosphoglycerate are used as variables. Also, the transition of the non-proliferative phase of diabetic retinopathy into the proliferative on the 180th day of the experiment was confirmed histologically. Results. We have developed a mathematical model for predicting the studied pathological state based on biochemical blood tests at the early stages of the experiment. We have proven the informative value of endothelial dysfunction markers, von Willebrand factor and endothelin-1, for predicting the transition of non-proliferative diabetic retinopathy into the proliferative phase. We determined the significance of a comprehensive analysis of the level of 2,3-diphosphoglycerate in erythrocytes together with the above markers of the functional status of the endothelium on day 30 for predicting the further course of the disease. Conclusions. We determined the effectiveness of a comprehensive analysis of the level of 2,3-diphosphoglycerate in erythrocytes together with the above markers of the functional status of the endothelium on day 30 for predicting the further course of the pathological process under study.
діабетична ретинопатія; прогнозування; математична модель; фактор Віллебранда; ендотелін-1; 2,3-дифосфогліцерат
диабетическая ретинопатия; прогнозирование; математическая модель; фактор Виллебранда; эндотелин-1; 2,3-дифосфоглицерат
diabetic retinopathy; prediction; mathematical model; von Willebrand factor; endothelin-1; 2,3-diphosphoglycerate
Introduction
Materials and methods
/96.jpg)
/96_2.jpg)
Results
/97.jpg)
/97_2.jpg)
/97_4.jpg)
Discussion
Conclusions
/98.jpg)
- Wang W., Lo A.C.Y. Diabetic Retinopathy: Pathophysiology and Treatments. Int. J. Mol. Sci. 2018. 19(6). 1816. doi: 10.3390/ijms19061816.
- Whitehead M., Wickremasinghe S., Osborne A., Van Wijngaarden P., Martin K.R. Diabetic retinopathy: a complex pathophysiology requiring novel therapeutic strategies. Expert Opin. Biol. Ther. 2018. 18(12). 1257-1270. doi: 10.1080/14712598.2018.1545836.
- Bandello F., Lattanzio R., Zucchiatti I., Del Turco C. Pathophysiology and treatment of diabetic retinopathy. Acta Diabetol. 2013. 50(1). 1-20. doi: 10.1007/s00592-012-0449-3.
- Tarr J.M., Kaul K., Chopra M., Kohner E.M., Chibber R. Pathophysiology of diabetic retinopathy. ISRN Ophthalmol. 2013. 2013. 343560. doi: 10.1155/2013/343560.
- Yau J.W., Rogers S.L., Kawasaki R., Lamoureux E.L., Kowalski J.W., Bek T., Chen S.J. et al. Meta-Analysis for Eye Disease (META-EYE) Study Group. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012. 35(3). 556-64. doi: 10.2337/dc11-1909.
- Romero-Aroca P., Baget-Bernaldiz M., Pareja-Rios A., Lopez-Galvez M., Navarro-Gil R., Verges R. Diabetic Macular Edema Pathophysiology: Vasogenic versus Inflammatory. J. Diabetes Res. 2016. 2016. 2156273. doi: 10.1155/2016/2156273.
- Gonzalez V.H., Campbell J., Holekamp N.M., Kiss S., Loewenstein A., Augustin A.J., Ma J. et al. Early and Long-Term Respon–ses to Anti-Vascular Endothelial Growth Factor Therapy in Diabetic Macular Edema: Analysis of Protocol I Data. Am. J. Ophthalmol. 2016. 172. 72-79. doi: 10.1016/j.ajo.2016.09.012.
- Bek T. Diameter changes of retinal vessels in diabetic retinopathy. Curr. Diabetes Rep. 2017. 17. 82. doi: 10.1007/s11892-017-0909-9.
- Nentwich M.M., Ulbig M.W. Diabetic retinopathy — ocular complications of diabetes mellitus. World J. Diabetes. 2015. 6(3). 489-99. doi: 10.4239/wjd.v6.i3.489.
- Karlberg C., Falk C., Green A., Sjølie A.K., Grauslund J. Proliferative retinopathy predicts nephropathy: a 25-year follow-up study of type 1 diabetic patients. Acta Diabetol. 2012. 49(4). 263-8. doi: 10.1007/s00592-011-0304-y.
- Kramer C.K., Retnakaran R. Concordance of retinopathy and nephropathy over time in type 1 diabetes: an analysis of data from the Diabetes Control and Complications Trial. Diabet. Med. 2013. 30(11). 1333-41. doi: 10.1111/dme.12296.
- Pasechnikova N.V., Moroz O.A. Protective action of quercetin and lipoate on functional groups of retinal proteins under simulated diabetes. Journal of Ophthalmology. 2015. 3. 76-81. doi: 10.31288/oftalmolzh201537681 (in Russian).
- Kaydash O.A., Ivanov V.V., Vengerovsky A.I., Buyko E.E., Schepetkin I.A. The experimental model of type 2 diabetes mellitus caused by a high-fat diet with low-dose streptozotocin in rats. Bulletin of Siberian Medicine. 2020. 19(2). 41-47. doi: 10.20538/1682-0363-2020-2-41-47 (in Russian).
- Reinhart K., Bayer O., Brunkhorst F., Meisner M. Markers of endothelial damage in organ dysfunction and sepsis. Crit. Care Med. 2002. 30(5, Suppl). S302-12. doi: 10.1097/00003246-200205001-00021.
- He S., Blombäck M., Wallén H., Jeppsson A., Grass S. Global impairments in the haemostasis systems after cardiopulmonary bypass. Thromb. Res. 2017. 151. 63-66. doi: 10.1016/j.thromres.2017.01.006.
- Marasciulo F.L., Montagnani M., Potenza M.A. Endothelin-1: the yin and yang on vascular function. Curr. Med. Chem. 2006. 13(14). 1655-65. doi: 10.2174/092986706777441968.
- Scott A.V., Nagababu E., Johnson D.J., Kebaish K.M., Lipsitz J.A., Dwyer I.M., Zuckerberg G.S. et al. 2,3-Diphosphoglycerate Concentrations in Autologous Salvaged Versus Stored Red Blood Cells and in Surgical Patients After Transfusion. Anesth. Analg. 2016. 122(3). 616-23. doi: 10.1213/ANE.0000000000001071.
- Nosko V.P. Econometrics. Book 2. Part 3, 4. M.: Publishing House “Delo”, 2011. 576 p. (in Russian).
- Basilevich K.A., Mazorchuk M.S., Sukhobrus A.A. Modelling in economy, arrangement of production and project management. Information Processing Systems. 2016. 2(139). 149-155 (in Russian).
- Sorrentino F.S., Matteini S., Bonifazzi C., Sebastiani A., Parmeggiani F. Diabetic retinopathy and endothelin system: microangiopathy versus endothelial dysfunction. Eye (Lond.). 2018. 32(7). 1157-1163. doi: 10.1038/s41433-018-0032-4.
- Siemianowicz K., Francuz T., Gminski J., Telega A., Syzdól M. Endothelium dysfunction markers in patients with diabetic retinopathy. Int. J. Mol. Med. 2005. 15(3). 459-62. PMID: 15702238.

/97_3.jpg)