Международный эндокринологический журнал Том 16, №3, 2020
Вернуться к номеру
COVID-19 and diabetes mellitus: management of patients during the pandemic
Авторы: N.V. Pashkovska(1), V.I. Pankiv(2), O.V. Pashkovska(3)
(1) — Bukovinian State Medical University, Chernivtsi, Ukraine
(2) — Ukrainian Research and Practical Centre of Endocrine Surgery, Transplantation of Endocrine Organs and Tissues of the Ministry of Health of Ukraine, Kyiv, Ukraine
(3) — Charles University in Prague, Prague, the Czech Republic
Рубрики: Эндокринология
Разделы: Справочник специалиста
Версия для печати
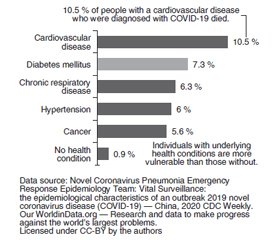
Коронавірусна хвороба 2019 (COVID-19) — потенційно тяжка гостра респіраторна інфекція, спричинена коронавірусом-2 (SARS-CoV-2), із вираженим гострим респіраторним синдромом. Люди з цукровим діабетом (ЦД) мають підвищений ризик виникнення серйозних розладів на тлі COVID-19. У статті повідомляється, що ЦД і неконтрольована глікемія є важливими предикторами тяжкості перебігу і смерті серед пацієнтів, інфікованих різними вірусами, включаючи пандемічний грип A (H1N1) у 2009 році, SARS-CoV і MERS-CoV. У триваючій пандемії SARS-CoV-2 у деяких дослідженнях не виявлено чіткого зв’язку між ЦД і тяжкістю захворювання. Однак аналіз даних із Китаю та Італії показав, що пацієнти похилого віку із хронічними захворюваннями, включаючи ЦД, зазнають більшого ризику тяжкої COVID-19 та смертності. Серед випадків смертності від COVID-19 в Ухані (Китай) основними супутніми захворюваннями були ЦД (42,3 %), артеріальна гіпертензія (53,8 %), захворювання серця в анамнезі (19,2 %) та церебральні розлади (15,4 %). Також смертність істотно зростає (на 6 %) за наявності ЦД (7,3 %) та інших супутніх захворювань, таких як серцево-судинні (10,5 %), хронічні захворювання органів дихання, артеріальна гіпертензія та рак. За даними досліджень, поширеність ЦД у людей, заражених вірусом, приблизно така ж, як і в загальній популяції, навіть дещо нижча. За результатами метааналізу 12 досліджень, які описують дані 2108 китайських пацієнтів із COVID-19, поширеність ЦД становила 10,3 %, що було аналогічно поширеності 10,9 % в 2013 році. Пацієнтам із ЦД рекомендується дотримуватися загальних порад щодо зменшення ризику зараження, а також специфічних для людей з ЦД. Усі сучасні рекомендації медичних організацій та наукових спільнот підкреслюють важливість належного контролю глікемії під час пандемії COVID-19, оскільки це може допомогти зменшити ризик зараження та тяжкість хвороби.
Коронавирусная болезнь 2019 (COVID-19) — потенциально тяжелая острая респираторная инфекция, вызванная коронавирусом-2 (SARS-CoV-2), с выраженным острым респираторным синдромом. Люди с сахарным диабетом (СД) имеют повышенный риск возникновения серьезных расстройств на фоне COVID-19. В статье сообщается, что СД и неконтролируемая гликемия являются важными предикторами тяжести и смерти среди пациентов, инфицированных различными вирусами, включая пандемический грипп A (H1N1) в 2009 году, SARS-CoV и MERS-CoV. В условиях продолжающейся пандемии SARS-CoV-2 в некоторых исследованиях не выявлено четкой связи между СД и тяжестью заболевания. Однако анализ данных из Китая и Италии показал, что пациенты пожилого возраста с хроническими заболеваниями, включая СД, имеют больший риск тяжелой COVID-19 и смертности. Среди случаев смертности от COVID-19 в Ухане (Китай) основными сопутствующими заболеваниями были СД (42,3 %), артериальная гипертензия (53,8 %), заболевания сердца в анамнезе (19,2 %) и церебральные расстройства (15,4 %). Также смертность существенно возрастает (на 6 %) при наличии СД (7,3 %) и других сопутствующих заболеваний, таких как сердечно-сосудистые (10,5 %), хронические заболевания органов дыхания, артериальная гипертензия и рак. По данным исследований, распространенность СД у людей, зараженных вирусом, примерно такая же, как и в общей популяции, даже несколько ниже. Согласно результатам метаанализа 12 исследований, которые описывают данные 2108 китайских пациентов с COVID-19, распространенность СД составила 10,3 %, что было аналогично распространенности 10,9 % в 2013 году. Пациентам с СД рекомендуется придерживаться общих советов по уменьшению риска заражения, а также специфических для лиц с СД. Все современные рекомендации медицинских организаций и научных сообществ подчеркивают важность надлежащего контроля гликемии во время пандемии COVID-19, так как это может помочь уменьшить риск заражения и тяжесть болезни.
Coronavirus disease 2019 (COVID-19) is a potentially severe acute respiratory infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). People with diabetes mellitus (DM) are at increased risk of serious illness from COVID-19. DM and uncontrolled glycemia were reported as significant predictors of severity and deaths in patients infected with different viruses, including the 2009 pandemic influenza A (H1N1), SARS-CoV and MERS-CoV. In the current SARS-CoV-2 pandemic, some studies did not find a clear association between DM and disease severity. However, other reports from China and Italy showed that older patients with chronic diseases, including DM, were at higher risk for severe COVID-19 and mortality. Among COVID-19 mortality cases in Wuhan, China, major associated comorbidities include DM (42.3 %), hypertension (53.8 %), previous heart disease (19.2 %) and cerebral infarction (15.4 %). Also, mortality strongly increased with the presence of DM (7.3 %) and other comorbidities like cardiovascular disease (10.5 %), chronic respiratory disease, hypertension and cancer, each at 6 %. According to several studies, the prevalence of DM in people infected with the virus is about the same as in the general population, even slightly lower. A meta-analysis of 12 studies describing data from 2,108 Chinese patients with COVID-19 reported a diabetes prevalence of 10.3 %, which was similar to the national prevalence of 10.9 % reported in 2013. Patients with DM are advised to follow general guidance on risk reduction and also specific to DM. All current recommendations of healthcare organizations and scientific communities emphasise the importance of good glycemic control during the COVID-19 pandemic as it may help in reducing the risk of infection and severity.
цукровий діабет; COVID-19
сахарный диабет; COVID-19
diabetes mellitus; COVID-19
Background
Current evidence
/8.jpg)
Measures in diabetic patients
Specific measures in diabetic patients
General preventive measures
Management of patients with diabetes mellitus and COVID-19
- Gupta R., Ghosh A., Singh A.K., Misra A. Clinical considerations for patients with diabetes in times of COVID-19 epidemic [published online ahead of print, 2020 Mar 10]. Diabetes Metab. Syndr. 2020. 14 (3). 211-212. doi: 10.1016/j.dsx.2020.03.002.
- Puig-Domingo M., Marazuela M., Giustina A. COVID-19 and endocrine diseases. A statement from the European Society of Endocrinology. Endocrine. 2020. 68. 2-5. doi: 10.1007/s12020-020-02294-5 (23 March 2020).
- Hartmann-Boyce J., Morris E., Goyder C. et al. Managing diabetes during the COVID-19 pandemic. The Centre for Evidence-Based Medicine develops, promotes and disseminates better evidence for healthcare: published online at cebm.net (April 8, 2020). Режим доступа: www.cebm.net/covid-19/managing-diabetes-during-the-covid-19-pandemic/
- Hussain A., Bhowmik B., Cristina do Vale Moreira N. COVID-19 and Diabetes: Knowledge in Progress [published online ahead of print, 2020 Apr 9]. Diabetes Res. Clin. Pract. 2020. 108142. doi: 10.1016/j.diabres.2020.108142.
- Zhang J.J., Dong X., Cao Y.Y. et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020. doi: 10.1111/all.14238 (23 February 2020).
- Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. doi: 10.1056/NEJMoa2002032 (29 February 2020).
- Wu Z., Mcgoogan J.M. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020. doi: 10.1001/jama.2020.2648 (24 February 2020).
- Onder G., Rezza G., Brusaferro S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA. 2020. doi: 10.1001/jama.2020.4683 (24 March 2020).
- Wang A., Zhao W., Xu Z., Gu J. Timely blood glucose management for the outbreak of 2019 novel coronavirus disease (COVID-19) is urgently needed [published online ahead of print, 2020 Mar 13]. Diabetes Res. Clin. Pract. 2020. 162. 108118. doi: 10.1016/j.diabres.2020.108118.
- Zhou J., Tan J. Diabetes patients with COVID-19 need better blood glucose management in Wuhan, China. Metabolism. 2020. 107. 154216. doi: 10.1016/j.metabol.2020.154216 (24 Mar 2020).
- Iqbal A., Prince L.R., Novodvorsky P. et al. Effect of Hypoglycemia on Inflammatory Responses and the Response to Low-Dose Endotoxemia in Humans. J. Clin. Endocrinol. Metab. 2019. 104 (4). 1187-1199. doi: 10.1210/jc.2018-01168 (1 April 2019).
- Li B., Yang J., Zhao F. et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China [published online ahead of print, 2020 Mar 11]. Clin. Res. Cardiol. 2020. 1-8. doi: 10.1007/s00392-020-01626-9.
- Fadini G.P., Morieri M.L., Longato E., Avogaro A. Prevalence and impact of diabetes among people infected with SARS-CoV-2. J. Endocrinol. Invest. 2020. doi: 10.1007/s40618-020-01236-2 (28 Mar 2020).
- Diabetes UK. Coronavirus and diabetes. Online at diabetes.org.uk (9 April 2020). Режим доступа: www.diabetes.org.uk/about_us/news/coronavirus
- International Diabetes Federation (IDF) Information on Corona-Virus Disease 2019 (COVID-19) outbreak and guidance for people with diabetes (15 April 2020). Режим доступа: www.idf.org/images/IDF_Europe/Information_on_Corona-Virus_Disease_2019__COVID-19_outbreak_and_guidance_for_people_with_diabetes_-_Final.pdf
- Goldenberg R.M., Berard L.D., Cheng A.Y.Y. et al. SGLT2 Inhibitor-associated Diabetic Ketoacidosis: Clinical Review and Recommendations for Prevention and Diagnosis. Clin. Ther. 2016. 38 (12). 2654-2664.e1. doi: 10.1016/j.clinthera.2016.11.002 (December 2016).
- Salpeter S., Greyber E., Pasternak G., Salpeter E. Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2002. 2. CD002967 (20 January 2010).
- Gordon D.E., Jang G.M., Bouhaddou M. et al. A SARS-CoV-2-Human Protein-Protein Interaction Map Reveals Drug Targets and Potential Drug-Repurposing (30 Mar 2020). Режим доступа: www.biorxiv.org/content/10.1101/2020.03.22.002386v3.full.pdf
- Song Z., Xu Y., Bao L., Zhang L., Yu P., Qu Y. From SARS to MERS, thrusting coronaviruses into the spotlight. Viruses. 2019. 11 (1). Epub 2019/01/17. doi: 10.3390/v11010059 (14 Jan 2019).
- Gentile S., Strollo F., Ceriello A. COVID-19 Infection in Italian people with diabetes: lessons learned for our future (an experience to be used). Diabetes Res. Clin. Pract. 2020. 108137. doi: 10.1016/j.diabres.2020.108137 (4 April 2020).
- Peng Y.D., Meng K., Guan H.Q., Leng L., Zhu R.R., Wang B.Y. Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV. Zhonghua Xin Xue Guan Bing Za Zhi. 2020. 48. E004. Epub 2020/03/04. doi: 10.3760/cma.j.cn112148-20200220-00105 (2 Mar 2020).
- World Health Organization (WHO). Coronavirus disease (COVID-19) advice for the public: Myth busters. Режим доступа: www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters