Резюме
Актуальність. Згідно з останніми дослідженнями, тиреоїдні гормони можуть мати потенційний вплив на ступінь тяжкості, перебіг та наслідки інсульту, але основні механізми цього зв’язку досі не вивчені. Мета дослідження: визначити вплив тиреоїдних гормонів на тяжкість неврологічного дефіциту при гострому ішемічному інсульті та ризик постінсультної інвалідизації. Матеріали та методи. До клінічного дослідження було залучено 168 дорослих пацієнтів із гострим ішемічним інсультом. Концентрації вільного трийодтироніну (fT3), вільного тироксину (fT4), тиреотропного гормону та основних факторів ризику інсульту визначали протягом 24 годин з моменту появи симптомів. Неврологічний дефіцит оцінювали за Скандинавською шкалою інсульту (SSS). Несприятливий результат інсульту (постінсультна інвалідизація) визначали як показник Модифікованої шкали Ренкіна ≥ 3 балiв через 6 місяців після інсульту. Результати. Статистичний аналіз ANOVA виявив, що показники SSS були значно вищими в пацієнтів із рівнем fT3 в 4-му квартилі (≥ 5,35 пмоль/л) порівняно з 2–3-м квартилем (медіана 48 балів проти 37, p = 0,0481) і особливо з 1-м квартилем (≤ 3,4050 пмоль/л, медіана 48 балів проти 30, р = 0,0018). У пацієнтів без інсульту в анамнезі (n = 124) рівень вільного трийодтироніну незалежно впливав на тяжкість неврологічного дефіциту за шкалою SSS (скорегований R2 = 0,49, p < 0,0001). Аналіз показав, що в пацієнтів з атеротромботичним підтипом інсульту (n = 108) рівень fT3 є незалежним фактором ризику несприятливого результату інсульту (відносний ризик = 0,3498, 95% довірчий інтервал 0,1235–0,9904). Згідно з ROC-аналізом, рівень fT3 < 4,44 пмоль/л був предиктором постінсультної інвалідизації (AUC = 0,727, специфічність — 96,4 %, чутливість — 66,8 %, p = 0,003). Висновки. Дослідження показало, що низький рівень трийодтироніну в сироватці крові під час дебюту інсульту негативно впливає на ступінь тяжкості в пацієнтів, які вперше перенесли інсульт, і може бути предиктором його несприятливого результату. У пацієнтів з атеротромботичним інсультом низький рівень вільного трийодтиронiну незалежно підвищував ризик постінсультної інвалідизації через 6 місяців. Для визначення можливих корисних ефектів додання трийодтиронiну як засобу нейропротекції під час інсульту необхідні майбутні дослідження.
Актуальность. Согласно последним исследованиям, тиреоидные гормоны могут иметь потенциальное влияние на степень тяжести, течение и последствия инсульта, но основные механизмы этой взаимосвязи до сих пор не изучены. Цель исследования: определить влияние тиреоидных гормонов на тяжесть неврологического дефицита при остром ишемическом инсульте и риск постинсультной инвалидизации. Материалы и методы. В клиническое исследование были включены 168 взрослых пациентов с острым ишемическим инсультом. Концентрации свободного трийодтиронина (fT3), свободного тироксина (fT4), тиреотропного гормона и основных факторов риска инсульта определяли в течение 24 часов с момента появления симптомов. Неврологический дефицит оценивали по Скандинавской шкале инсульта (SSS). Неблагоприятный исход инсульта (постинсультная инвалидизация) определяли как показатель модифицированной шкалы Рэнкина ≥ 3 баллов через 6 месяцев после инсульта. Результаты. Статистический анализ ANOVA выявил, что показатели SSS были значительно выше у пациентов с уровнем fT3 в 4-м квартиле (≥ 5,35 пмоль/л) по сравнению со 2–3-м квартилем (медиана 48 баллов против 37, p = 0,0481) и особенно с 1-м квартилем (≤ 3,4050 пмоль/л, медиана 48 баллов против 30, р = 0,0018). У пациентов без инсульта в анамнезе (n = 124) уровень свободного трийодтиронина независимо влиял на тяжесть неврологического дефицита по шкале SSS (скорректированный R2 = 0,49, p < 0,0001). Анализ показал, что у пациентов с атеротромботическим подтипом инсульта (n = 108) уровень fT3 является независимым фактором риска неблагоприятного исхода инсульта (относительный риск = 0,3498, 95% доверительный интервал 0,1235–0,9904). Согласно ROC-анализу, уровень fT3 < 4,44 пмоль/л был предиктором постинсультной инвалидизации (AUC = 0,727, специфичность — 96,4 %, чувствительность — 66,8 %, p = 0,003). Выводы. Исследование показало, что низкий уровень трийодтиронина в сыворотке крови во время дебюта инсульта негативно влияет на степень тяжести у пациентов, впервые перенесших инсульт, и может быть предиктором его неблагоприятного исхода. У пациентов с атеротромботическим инсультом низкий уровень свободного трийодтиронина независимо повышал риск постинсультной инвалидизации через 6 месяцев. Для определения возможных полезных эффектов добавления трийодтиронина как средства нейропротекции во время инсульта необходимы будущие исследования.
Background. According to recent studies, thyroid hormones may have various effects on stroke severity, course and outcome, but underlying mechanisms of this association are still unclear. The purpose was to determine the relationship of thyroid hormones during stroke onset with stroke severity and outcome in a clinical study. Materials and methods. In this study, 168 adult patients with acute ischemic stroke were enrolled. Concentrations of free triiodothyronine (fT3), free thyroxine (fT4), thyroid-stimulating hormone and basic stroke risk factors were assessed during 24 h from symptoms onset. Neurological deficit was evaluated by Scandinavian Stroke Scale (SSS). Disabling deficit was defined as Modified Rankin Scale score ≥ 3 points six months after stroke. Results. ANOVA showed that SSS scores were significantly higher in patients with fT3 level in quartile IV (≥ 5.35 pmol/l) compared to quartiles II–III (SSS median 48 vs. 37, p = 0.0481) and especially to quartile I (≤ 3.4050 pmol/l, SSS median 48 vs. 30, p = 0.0018). In patients without prior stroke (n = 124), fT3 independently affected baseline SSS score (corrected R2 = 0.49, p < 0.0001). The analysis showed that in patients with atherothrombotic stroke subtype (n = 108), fT3 level was an independent risk factor for unfavourable stroke outcome (odds ratio = 0.3498, 95% confidence interval 0.1235–0.9904). According to ROC-analysis, fT3 level < 4.44 pmol/l was a predictor of disabling deficit (AUC = 0.727, specificity — 96.4 %, sensitivity — 66.8 %, p = 0.003). Conclusions. The study showed that a low serum free triiodothyronine level during stroke onset negatively affects the stroke severity in first stroke patients and may be a predictor of its unfavourable outcome. In patients with atherothrombotic stroke, lower baseline fT3 levels were independently associated with poor outcome after 6 months. Beneficial effects of additional fT3 supplement during stroke should be assessed in future studies.
Introduction
According to statistics over the past decade, mortality from cardiovascular diseases invariably ranks first in the world, although in certain countries of Europe and in the United States there is some stabilization of growth dynamics [1]. During recent years, governments of many countries have significantly strengthened preventive measures aimed at reducing the frequency of risk factors for cerebrovascular pathologies. Although the growth in the number of strokes slowed down, this pathology still remains one of the most common causes of death in Europe, North America and Asia.
The results of several controlled randomized trials of treatment in hyperacute stroke phase were published in recent years. All studies have confirmed the obvious advantage of an integrated approach in the treatment of acute ischemic stroke caused by thrombotic occlusion of the intracranial arteries of the carotid system. This approach consists of using a combination of systemic thrombolysis and endovascular thrombectomy in the first few hours after the onset of the first symptoms of acute stroke [2, 3]. However, reperfusion therapy is possible only within a relatively narrow therapeutic window [4]. In cases where thrombolysis or thrombectomy is not indicated or there are no opportunities for its implementation, approaches to patient’s management du-ring the acute period of stroke include both secondary prevention of cerebrovascular disease and an attempt to reduce the severity of neurological deficit by protecting ischemic (but potentially viable) brain tissue in penumbra zone [5]. Nevertheless, despite the diversity of neuroprotective drugs, different in their mechanism of action and effective in preclinical studies, none of them has enough clinical efficacy. In this regard, the search for new approaches to neuroprotection remains one of the most important tasks of modern neuropharmacology [5].
The survival of the brain tissue under ischemia depends on the intensity of metabolism, oxygen demand, as well as the ability to maintain the redox potential and support the synthesis of high-energy compounds (adeno-sine triphosphate (ATP), etc.). The mechanism of action of most neuroprotectors is based on the effects on these processes [6, 7].
Over the past decades, special attention was paid to the neuroprotective properties of endogenous molecules such as vascular endothelial growth factor, erythropoietin, brain-derived neurotrophic factor, etc. It is known that triiodothyronine, an active form of the thyroid hormone thyroxin, separates tissue respiration and oxidative phosphorylation. This process leads to disruption of the Krebs cycle, reduced ATP production, hyperthermia, and has a potentially negative effect in acute cerebral ischemia [8]. On the other hand, it is known that triiodothyronine has several neuroprotective effects: it contributes to the uptake of neurotoxic glutamate by astrocytes, stimulation of the Na+/K+ membrane channels in neurons, the restoration of intracellular pH [9]. Thus, selective therapeutic effect on thyroid metabolism (stimulation or inhibition of the function of thyroid hormones) may be promising potential target for new approaches to the treatment of stroke.
In recent years, more publications appeared in the lite-rature about the possible effect of thyroid hormones on the risk of development, severity and outcome of acute ischemic stroke. Nevertheless, the results of the published works are rather contradictory [10]. Finally, the nature of the influence of hyper- or hypothyroidism on the course and outcome of a stroke is still unclear.
The purpose of this study was to determine the relationship between markers of thyroid function and the severity of neurological and functional deficit in acute ischemic stroke.
Materials and methods
This study was conducted at the single clinical and research center — V.K. Gusak Institute of Urgent and Reparative Surgery. One hundred and sixty-eight patients (71 women, 97 men) aged 42 to 78 years with acute ischemic heterogeneous stroke were enrolled in this study. Patients with verified autoimmune thyroiditis or a malignancy were excluded from the study. Within 24 hours from stroke onset, basic risk stroke factors were analyzed. Serum free triiodothyronine (fT3), free thyroxine (fT4) and thyroid-stimulating hormone (TSH) were determined using enzyme-linked immunosorbent assay (ChemWell EIA analyzer with DRG International kits). Blood sampling was performed during 24 hours from stroke onset. Neurological deficit was assessed using Scandinavian Stroke Scale (SSS). Poor stroke outcome was assumed as 3 or more points on the modified Rankin Scale (mRs) 6 months after stroke onset. Thyroid hormones and TSH levels below 25th and above 75th percentile were considered low and high, respectively.
Statistical analysis was performed using MedCalc v14 software. Continuous data with non-normal distribution are presented as median and 95% confidence interval (CI). Analysis of variation (ANOVA) was used to evaluate the degree of neurological deficit, and patients were divided to subgroups according to T3 levels: hypothyroid (T3 below 25th percentile), euthyroid (T3 in 25–75th
percentile), hyperthyroid (T3 above 75th percentile). For determining the impact of thyroid hormones on stroke outcome using logistic regression, patients were divided into subgroups with good (mRs 0–2) and poor outcome (mRs 3–6).
Results
Strokes in the carotid territory were the most frequent (79 %), with the atherothrombotic subtype being the most common (64 %). The leading basic risk factors were arterial hypertension (65 %), smoking (42 %), ischemic heart disease (29 %), atrial fibrillation (27 %). Forty-nine patients (28 %) had history of transient ischemic attack (TIA) or ischemic stroke, 119 people had the ischemic stroke deve-loped for the first time. Demographic characteristics of the examined patients are presented in Table 1.
According to the laboratory reference indicators, 112 patients had thyroid hormones levels in the reference range, 36 individuals had laboratory hypothyroidism, and 20 — laboratory hyperthyroidism. Thyroid hormones levels are presented in Table 2.
/63_2.jpg)
Correlation analysis using the Spearman rank correlation revealed a positive statistically significant relationship between the level of free triiodothyronine and the severity of neurological deficit according to the SSS. A statistically significant relationship was also found between the level of free thyroxine and the presence of atrial fibrillation. Among other factors, an inverse correlation was observed between the level of C-reactive protein (CRP) and the severity of neurological deficit according to the SSS (R = –0.397, p = 0.0004). No other significant correlation was found between thyroid hormones, severity of neurological deficit, and the presence of basic risk factors for stroke. The results of the correlation analysis are presented in Table 3.
ANOVA showed that patients with fT3 level in quartile IV (≥ 5.35 pmol/l; 95% CI 5.01–5.61) had less severe stroke (higher SSS scores) compared to those with fT3 level in quartile II–III (SSS median is 48 vs 37 points, respectively; p = 0.0481), and especially compared to people whose T3 level was in quartile I (≤ 3.4050 pmol/l, SSS median is 48 vs 30 points; p = 0.0018). The results of the ANOVA are presented in Fig. 1.
The results of ANOVA suggest that low triiodothyronine levels are associated with a more severe neurological deficit, while high levels may have potential neuroprotective effects. There were no statistically significant variations of SSS score in subgroups of patients according to fT4 or TSH levels.
After 6 months, 120 patients were classified as those having stroke with poor outcome and 48 patients had stroke with favourable outcome. Comparative analysis showed that patients with poor outcome were older, had significantly lower fT3, higher CRP levels and lower free T3 to free T4 ratio.
To clarify the relationship between the severity of neurological deficit and the level of free triiodothyronine in serum, a regression analysis was performed. Univariate regression analysis showed that in patients with cardioembolic stroke, fT4 favourably influenced the severity of the stroke according to the SSS (R2 = 0.75, p = 0.0005), but this association weakened after adjustment for other stroke risk factors (age, hypertension, carotid stenosis, glucose level, C-reactive protein, SSS score).
Univariate regression showed no relationship between the severity of neurological deficit and the level of triiodothyronine. However, after exclusion of patients with previous stroke, a regression dependence of the severity of neurological deficit on the level of free triiodothyronine was detected (F = 15.7920, p = 0.0002, corrected R2 = 0.44).
There were no significant differences in thyroid hormones levels, CRP and SSS score in patients with the first stroke and people with history of stroke or TIA.
To confirm the independent effect of fT3 level on the seve-rity of stroke and exclude the influence of co-factors, a multivariate regression analysis was performed. The regression model included basic risk stroke factors (age, arterial hypertension, blood pressure at admission, atrial fibrillation, ischemic heart disease, diabetes, smoking), C-reactive protein, free thyroxine, TSH levels, free T3 to free T4 ratio. Variables were introduced in the regression model using the forward method.
Multivariate regression analysis showed that the independent factors affecting the severity of neurological deficit in patients with no prior stroke were the levels of free triiodothyronine (p = 0.0035) and of C-reactive protein (p = 0.0035). Model had the coefficient of variation F = 17.45 (p < 0.0001) and corrected R2 = 0.49. The obtained results confirmed the independent effect of serum free triiodothyronine level on the severity of neurological deficit in newly developed ischemic stroke, while the low levels of triiodothyronine were associated with more severe stroke.
To assess the impact of fT3 level on stroke outcome, the multiple logistic regression method was used. Basic stroke risk factors (age, hypertension, blood pressure at admission, atrial fibrillation, coronary artery disease, diabetes mellitus, smoking), C-reactive protein, free thyroxine, TSH levels, fT3/fT4 ratio were included in the regression model. Lower fT3 levels were independently associated with poor stroke outcome (odds ratio (OR) = 0.3408, 95% CI 0.15–0.77), but this association became insignificant after correction for baseline SSS score.
When multiple logistic regression included only patients with atherothrombotic stroke, the analysis showed that fT3 level was an independent risk factor for unfavourable stroke outcome even after correction for baseline SSS score (OR = 0.3498, 95% CI 0.1235–0.9904). Independent factors are demonstrated in Table 5.
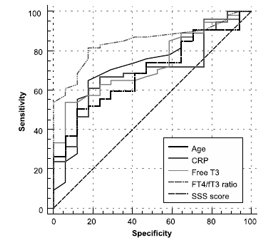
In order to determine the critical values of free triiodothyronine associated with the greatest risk of poor stroke outcome, the analysis of receiver operating characteristic (ROC) curves was applied. It was found that fT3 level < 4.44 pmol/l is a predictor of poor stroke outcome (area under ROC-curve = 0.727, specificity — 96.4 %, sensitivity — 66.8 %, p = 0.003). The results of the analysis of ROC-curves are presented in Fig. 2.
Discussion
The results of this study indicate that low serum free triiodothyronine level during stroke onset is associated with a more severe neurological deficit in a patient with first ischemic stroke. The difference between this and equivalent studies is the identification of independent influence of free triiodothyronine on the stroke severity in multivariate regression analysis. There are several limitations in this study. The main disadvantages are lack of long-term follow-up and inability to use Cox regression method.
This study was underpowered to reveal the independent influence of low free triiodothyronine level on poor stroke outcome in all stroke subtypes. Nevertheless, obtained data showed that in patients with atherothrombotic stroke subtype, lower baseline fT3 levels were independently associated with poor outcome. This association may be attributed to endothelium dysfunction, hyperhomocysteinemia and possibly other mechanisms, which are observed in atherothrombotic stroke subtype.
Our results correlate with the fundamental research carried out in recent years. In experimental models, it has been shown that the administration of L-thyroxin after transient cerebral ischemia contributes to an increase in neuron density and stimulation of angiogenesis in the ischemic brain [11]. The results of another in vitro study revealed that triiodothyronine can restore intracellular concentration of sodium, calcium ions and pH [8]. It was shown that thyroxine stimulates the synthesis of other neurotrophic factors, such as fibroblast growth factor [12].
Several clinical studies also confirm experimental data. L.M. O’Keefe et al. in a study of 868 patients with heterogeneous ischemic stroke found that a low triiodothyronine level was associated with greater functional deficiency 3 months after a stroke and with higher nosocomial mortality [13]. Results of another study of 833 patients with acute ischemic stroke indicate that low levels of total triiodothyronine (even within the reference range) were associated with poor stroke outcome [14].
In the first hours after disturbance of cerebral blood flow in neurons in the affected area, ATP pool depletion, inhibition of protein synthesis, and an intracellular pH shift to the acidic side are observed. Excessive release of excitatory and inhibitory neurotransmitters, especially glutamate, leads to the development of the excitotoxicity. Activation of ionotropic and metabotropic glutamate receptors increases the cytosolic level of calcium ions. In turn, an excess of calcium ions disrupts the function of ion pumps and simultaneously activates many catabolic enzymes, resulting in depolarization and disintegration of the intracellular membranes. The destruction of mitochondrial membranes involves apoptosis by the release of proapoptotic proteins.
Some experimental studies demonstrated that after the addition of T3 in in vivo astrocyte culture, the number of glutamate transporters (glutamate transporter-1 and glutamate aspartate transporter) increased. Activation of glutamate uptake by astrocytes significantly reduced the gliotoxic effect of this neurotransmitter for neurons [23]. In another experiment, it was revealed that triiodothyronine reduced the activity of N-methyl-D-aspartate receptors in hippocampal neurons, which, according to the authors, prevented glutamate-induced cell death [24].
The key role of iodothyronines in the synthesis and stimulation of ion exchange pumps has been proved. So, T3 activates the expression of the sodium/hydrogen exchanger gene, which, in turn, is responsible for removing excess protons and normalizing intracellular pH. Under the action of T3, the number of Na/K-ATPases integrated into the membranes increases, the functioning of Ca2+-ATPases increases, which ultimately contributes to the normalization of the ion balance of neurons [25].
Normal work of ion pumps is not possible under conditions of ATP pool depletion in cells against ischemia. When studying the effect of T3 on astrocyte cultures, an increase in the expression of palmitate beta-oxidation enzymes in mitochondria: beta-hydroxyacyl-CoA dehydrogenase, beta-thiolase, and enoyl-CoA hydratase was recorded [26]. As a result, the amount of ATP in astrocytes increased. Since the protective role of these cells in stroke is considered to be proven, the authors of the study concluded that there was the normalization of energy exchange under the action of triiodothyronine in astrocytes that significantly reduced the lesion area in experimental models of transient cerebral ischemia and stroke.
A comparison of two experimental models of ischemic stroke, with transient and permanent occlusion, revealed another important feature of the neuroprotective effect of T3 — inhibition of protein aquaporin-4 synthesis in transient occlusion [27]. As a result of treatment of experimental animals with triiodothyronine preparations, a marked decrease in swelling and the area of brain damage was observed, the probability of a favourable outcome increased, but only in the model of transient ischemia.
Nevertheless, the biological basis of the association of hypothyroidism with the stroke course and outcome has not been finally studied. In this context, researches of new class of thyroid hormones — thyronamines (decarboxylated triiodothyronine derivatives) seems promising. These substances are a new class of endogenous signaling hormones that exhibit significant in vivo effects, such as:
1) decrease in the rate of basal metabolism, decrease in respiratory rate [15];
2) fast, deep and reversible hypothermia [16];
3) weight loss [17];
4) negative inotropic and chronotropic effects without changing the absorption of glucose and oxygen [18];
5) decrease in Ca2+ level in the endoplasmic reticulum [19];
6) ischemia resistance [20];
7) increase in high-energy compounds level in target cells [21].
Thyronamines have a wide range of potential neuroprotective effects, the most significant of which are induction of hypothermia and a decrease in the rate of basal metabolism. According to K.P. Doyle et al., intraperitoneal administration of thyronamines to laboratory mice contributes to a decrease in body temperature from 37 to 31 °C, and significantly reduces the infarction zone after transient cerebral ischemia. At the same time, the observed hypothermia is completely reversible, and is not accompanied by any side effects, and its development is not associated with the effects of the known mechanisms of thermoregulation [22].
It is noteworthy that thyronamines, being derivatives of L-thyroxin, have antagonistic properties in relation to it, and the metabolic effects of thyronamines are close to the effects observed in hypothyroidism. It is possible that this phenomenon is the basis for the neuroprotective effects of thyroid hormones.
To confirm the neuroprotective effects of thyronamines, analogue of T0AM (thyronamine) was synthesized by our colleagues from the L.M. Litvinenko Institute of Physical Organic Chemistry and Coal Chemistry (Donetsk, Donbass region) for research in animal experimental model. Preliminary results showed that injection of T0AM at a dose of 50 mg/kg to laboratory rats prevents a reduction in superoxide dismutase levels after brain ischemia and also leads to a significant reversible body temperature decrease of 2.5 °C. Currently, the study of the thyronamine neuroprotective properties in the experimental stroke model is ongoing at our institute.
Even though in recent years more and more evidence has been obtained on the influence of thyroid hormones on risk, course and outcome of cerebrovascular disease, the nature and biological basis of this relationship have not been finally identified. This was the reason for initiation in our institute of a complex clinical and experimental trial on the study of the possibility of using thyroid hormones and their derivatives as neuroprotective therapy in acute ischemic stroke.
Conclusions
The study showed that a low serum free triiodothyronine level during stroke onset negatively affects the stroke severity in patients with the first stroke and may be a predictor of its unfavourable outcome. In patients with atherothrombotic stroke subtype, lower baseline fT3 levels were independently associated with poor outcome. The findings suggest that thyroid metabolism is not only a factor affecting the course of ischemic stroke, but also a potential target for therapeutic correction. To confirm the effectiveness of this approach, it is necessary to conduct further clinical and experimental studies. It is reasonable to monitor thyroid hormones levels during stroke, while the analysis of serum free triiodothyronine can be used to predict a high risk of an unfavourable stroke outcome. Researches to determine possible beneficial effects of additional T3 supplement in ischemic stroke patients are ongoing at out institute.
Conflicts of interests. Authors declare the absence of any conflicts of interests and their own financial interest that might be construed to influence the results or interpretation of their manuscript.
Список литературы
1. Stroke Association. State of the Nation: Stroke Statistics 2015. State of the Nation. 2015 Jan. 39. Available from: https://www.stroke.org.uk/sites/default/files/stroke_statistics_2015.pdf.
2. IST-3 collaborative group. Sandercock P., Wardlaw J.M., Lindley R.I., Dennis M., Cohen G. et al. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet. 2012 Jun 23 [cited 2020 Feb 16]. 379(9834). 2352-63. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22632908.
3. Bhaskar S., Stanwell P., Cordato D., Attia J., Levi C. Reperfusion therapy in acute ischemic stroke: dawn of a new era? BMC Neurology. 2018 [cited 2020 Feb 16]. 18. 8. Available from: https://bmcneurol.biomedcentral.com/articles/10.1186/s12883-017-1007-y.
4. Boyle K., Joundi R.A., Aviv R.I. An historical and contemporary review of endovascular therapy for acute ischemic stroke. Neurovascular Imaging. 2017 Dec 27 [cited 2020 Feb 16]. 3(1). 1. Available from: http://nvijournal.biomedcentral.com/articles/10.1186/s40809-016-0025-2.
5. Liu R., Yuan H., Yuan F., Yang S.H. Neuroprotection targeting ischemic penumbra and beyond for the treatment of ischemic stroke. Neurological Research. 2012 [cited 2020 Feb 16]. 34. 331-7. Available from: https://www.tandfonline.com/doi/full/10.1179/1743132812Y.0000000020.
6. Ramos-Cabrer P., Campos F., Sobrino T., Castillo J. Targeting the ischemic penumbra. Stroke. 2011. 2442-56.
7. Boltze J., Kleinschnitz C., Reymann K.G., Reiser G., Wagner D.-C., Kranz A. et al. Neurovascular pathophysiology in cerebral ischemia, dementia and the ageing brain — current trends in basic, translational and clinical research. Exp. Transl. Stroke Med. 2012 Jan [cited 2015 Mar 23]. 4(1). 14. Available from: http://www.etsmjournal.com/content/4/1/14.
8. Lin H.-Y., Davis F.B., Luidens M.K., Mousa S.A., Cao J.H., Zhou M. et al. Molecular basis for certain neuroprotective effects of thyroid hormone. Front. Mol. Neurosci. 2011 [cited 2017 Mar 19]. 4. 29. Available from: http://journal.frontiersin.org/article/10.3389/fnmol.2011.00029/abstract.
9. Bunevicius A., Iervasi G., Bunevicius R. Neuroprotective actions of thyroid hormones and low-T3 syndrome as a biomarker in acute cerebrovascular disorders. Expert Rev. Neurother. 2015 Mar 4 [cited 2017 Mar 19]. 15(3). 315-26. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25673072.
10. Forti P., Maioli F., Coveri M., Nativio V., Arnone G., Loreti A. et al. Thyroid function tests and early outcomes of acute ische-mic stroke in older euthyroid patients. Exp. Gerontol. 2015 Jan [cited 2017 Apr 5]. 61. 8-14. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0531556514003106.
11. Schlenker E.H., Schultz H.D. Hypothyroidism stimulates D2 receptor-mediated breathing in response to acute hypoxia and alters D2 receptors levels in carotid bodies and brain. Respir. Physiol. Neurobiol. 2012 Jan 15 [cited 2017 Sep 15]. 180(1). 69-78. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22051191.
12. Sadana P., Coughlin L., Burke J., Woods R., Mdzinarishvili A. Anti-edema action of thyroid hormone in MCAO model of ischemic brain stroke: possible association with AQP4 modulation. J. Neurol Sci. 2015. 354(1–2). 37-45.
13. O’Keefe L.M., Conway S.E., Czap A., Malchoff C.D., Benashski S., Fortunato G. et al. Thyroid hormones and functional outcomes after ischemic stroke. Thyroid Res. 2015 [cited 2017 Mar 19]. 8(1). 9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26157487.
14. Xu X.Y., Li W.Y., Hu X.Y. Alteration of thyroid-related hormones within normal ranges and early functional outcomes in patients with acute ischemic stroke. Int. J. Endocrinol. 2016 [cited 2017 Sep 15]. 2016. 1-5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27375741.
15. Scanlan T.S., Suchland K.L., Hart M.E., Chiellini G., Huang Y., Kruzich P.J. et al. 3-iodothyronamine is an endogenous and rapid-acting derivative of thyroid hormone. Nat. Med. 2004 Jun [cited 2017 Sep 15]. 10(6). 638-42. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15146179.
16. Venditti P., Napolitano G., Di Stefano L., Chiellini G., Zucchi R., Scanlan T.S. et al. Effects of the thyroid hormone derivatives 3-iodothyronamine and thyronamine on rat liver oxidative capacity. Mol. Cell. Endocrinol. 2011. 341(1–2). 55-62.
17. Piehl S., Hoefig C.S., Scanlan T.S., Köhrle J. Thyronamines — past, present, and future. Endocr. Rev. 2011. 32(1). 64-80.
18. Cichero E., Tonelli M. New insights into the structure of the trace amine-associated receptor 2: homology modelling studies exploring the binding mode of 3-iodothyronamine. Chem. Biol. Drug Des. 2017. 89(5). 790-6.
19. Chiellini G., Frascarelli S., Ghelardoni S., Carnicelli V., Tobias S.C., DeBarber A. et al. Cardiac effects of 3-iodothyronamine: a new aminergic system modulating cardiac function. FASEB J. 2007. 21(7). 1597-608.
20. Kinne A., Kleinau G., Hoefig C.S., Grüters A., Köhrle J., Krause G. et al. Essential molecular determinants for thyroid hormone transport and first structural implications for monocarboxylate transporter 8. J. Biol. Chem. 2010 Sep 3 [cited 2019 Sep 22]. 285(36). 28054-63. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20628049.
21. Panas H.N., Lynch L.J., Vallender E.J., Xie Z., Chen G.L., Lynn S.K. et al. Normal thermoregulatory responses to 3-iodothyronamine, trace amines and amphetamine-like psychostimulants in trace amine associated receptor 1 knockout mice. J. Neurosci. Res. 2010. 88(9). 1962-9.
22. Doyle K.P., Suchland K.L., Ciesielski T.M.P., Lessov N.S., Grandy D.K., Scanlan T.S. et al. Novel thyroxine derivatives, thyronamine and 3-iodothyronamine, induce transient hypothermia and marked neuroprotection against stroke injury. Stroke. 2007 [cited 2017 Sep 15]. 38(9). 2569-76. Available from: http://stroke.ahajournals.org/content/strokeaha/38/9/2569.full.pdf.
23. Mendes-de-Aguiar C.B., Alchini R., Decker H., Alvarez-Silva M., Tasca C.I., Trentin A.G. Thyroid hormone increases astrocyte glutamate uptake and protects astrocytes and neurons against glutamate toxicity. J. Neurosci. Res. 2008. 86. 3117-3125.
24. Losi G., Garzon G., Puia G. Nongenomic regulation of glutamatergic neurotrans mission in hippocampus by thyroid hormones. Neuroscience. 2008. 151. 155-163.
25. Lin H.-Y., Davis F.B., Luidens M.K., Mousa S.A., Cao J.H., Zhou M. et al. Molecular basis for certain neuroprotective effects of thyroid hormone. Frontiers in Molecular Neuroscience. 2011 Oct. 4. Article 29.
26. Sayre N.L., Sifuentes M., Holstein D., Cheng S.-Y., Zhu X., Lechleiter J.D. Stimulation of astrocyte fatty acid oxidation by thyroid hormone is protective against ischemic stroke-induced damage. Journal of Cerebral Blood Flow & Metabolism. 2017. 37(2). 514-52.
27. Sadana P., Coughlin L., Burke J., Woods R., Mdzinarishvili A. Anti-edema action of thyroid hormone in MCAO model of ischemic brain stroke: possible association with AQP4 modulation. Journal of the Neurological Sciences. 2015. doi: 10.1016/j.jns.2015.04.04.
/62.jpg)
/63.jpg)
/64.jpg)

/63_2.jpg)
/64_2.jpg)