Introduction
Benign recurrent lymphocytic meningitis, or Mollaret meningitis (MM), is a disease characterized by headache, fever and vomiting; in 84 % of cases, it is caused by the reactivation of type 2 herpes simplex virus (HSV) with or without genital rashes [1].
Headache is one of the most common pathological conditions. Thus, according to epidemiological studies, 45 % of the adult population has ever reported severe or disabling cephalgia. According to the World Health Organization, from half to three quarters of people aged 18–65 years in the world have had a headache over the past year. 1.7–4 % of the world’s adult population suffers from a headache that lasts 15 or more days every month. Despite the differences in regions, headache is a worldwide problem affecting peop–le regardless of age, race, income level and geographical area that violate their domestic and professional activities [2, 4]. Diagnosis is complicated by various clinical manifestations, hundreds of different etiologies, both benign and life-threatening, which cause a headache. In recent years, there has been a transformation in the understanding of etiopathogenesis, classification, diagnosis and treatment of headaches, which helps doctors better understand this problem, and improve the quality of life of patients [3]. The problem of diagnosis and treatment of headache remains interdisciplinary, often requiring the participation of many specialists (neurologist, ophthalmologist, infectious disease specialist, general practitioner, maxillofacial surgeon, etc.) [5]. One of headache causes is infection due to persistent viruses, in particular, herpes simplex virus (HSV) infection type 1 + 2, which is facilitated by their ubiquity [6]. Thus, the issues of diagnosis and successful treatment of recurrent headaches are of great scientific and practical importance.
Presentation of clinical cases
Patient Sh., 47 years old, a resident of the city of Dnipro, an ethnic Slavic woman, came to the clinic with complaints of severe headache that started three days ago and still continues at the time of the examination, accompanied by genital rash, as well as weakness and low grade fever.
From the patient’s life history: socially adapted, has two healthy daughters aged 12 and 22 years. The patient categorically denies the use of alcohol, drugs, and any medicinal psychotropic drugs. For twenty years (with sexual debut) she suffers a persistent headache, which causes increased fatigue and mood swings. According to the patient, increased attacks of cephalalgia arose about 12 years ago, after giving birth the second time, and the subsequent surgery and chemotherapy for malignant papilloma of the uterus. Since this time, attacks of severe headaches began to combine with genital vesicles on the labia majora, and in the last few years, there have been 7 to 9 such episodes per year. The duration of these episodes ranged from 4 to 7 days, during which the headache, as the patient described, had a persistent severe nature. At the same time, the fever was insignificant, short-term and did not combine with signs of any systemic disease. During episodes of genital rash, the patient irregularly and in inappropriate doses took acyclovir (Ac) orally.
According to the epidemiological history, the vesicular rash on the genitals took place in previous marriage. The patient did not perform laboratory studies of the contents of genital vesicles, a priori believing that they were manifestations of HSV.
Clinical status. When examining the patient, the gene–ral condition was satisfactory. Vital signs are within normal limits. Body mass index is 23 kg/m2. Skin has natural color, there is no rash or enanthema on the oral mucosa; some benign spots of the lentigo type are seen. All groups of peripheral lymph nodes are not enlarged. No pathology of cardiorespiratory and digestive systems is revealed. Li–ver and spleen are of normal size and density. Neurological exa–mination detected no deficiency of the peripheral nerve function. Appearance and mobility of muscles and joints are without pathological findings.
Considering the severity of headache, as well as the pre–sence of vesicular genital rash, the patient was recommended to be hospitalized and was discharged in 3 days. In the hospital, routine blood and urine tests, frontal lung radio–graphy were performed, and no abnormalities were detected. The blood test for antibodies to human immunodeficiency virus-1 (HIV-1) using enzyme-linked immunosorbent assay (ELISA) was negative. Spinal puncture conducted on day 8 from the onset of the headache attack and vesicular rash showed a clear liquor: cells — 2 lymphocytes in 1 μl, glucose — 2.2 mmol/l, protein level — 0.12 g/l. Analysis of cerebrospinal fluid (CSF) for the presence of HSV 1 + 2 –deoxyribonucleic acid (DNA), cytomegalovirus (CMV) and Epstein-Barr virus (EBV) by the polymerase chain reaction (PCR) did not reveal the genetic material of these pathogens. In the blood serum, G class antibodies to HSV 1 + 2 type, CMV and EBV nuclear antigen were detected by the ELISA. Analysis of vaginal content for HSV 1 + 2 DNA by PCR was not carried out, because by this time, vesicular rash had disappeared.
Despite the absence of HSV DNA and signs of inflammation following cerebrospinal fluid (CSF) analysis, acyclovir was administered intravenously as an infusion for 1 hour at a dose of 500 mg 3 times a day (every 8 hours) for 7 days, after which the patient was switched to the oral valacyclovir (VAc) at a dose of 1,000 mg/day. The choice of this dose of VAc is proved by the fact that in the presence of more than 9 episodes of genital herpes for systemic suppressive antiviral chemotherapy, 1,000 mg of the drug is recommended daily, for an indefinitely long time [7]. The choice of VAc was determined by a higher enteric bioavailability of the drug, compared with acyclovir, convenient compliance (one dose per day), and an optimal safety profile — side effects are rare. During examination on 18.03.17, after 5 months of continuous administration of VAc at a dose of 1,000 mg/day 1 time in the morning, the patient states a significant improvement in the well-being: the amount and severity of cephalgia decreased, the emotional tone improved, the relapses of genital rash decreased (noted once, after freezing in a swimming pool). Given the relationship between the appearance of disease symptoms and a decrease in the environmental temperature, it was decided that until April, the patient takes 1,000 mg/day with the subsequent complete permanent drug discontinuation. At the same time, it was stipulated with the patient that in case of genital rash relapse, regardless of the presence or absence of cephalgia, the dose of VAc imme–diately increases to 3,000 mg/day (1,000 mg in three divided doses).
Discussion
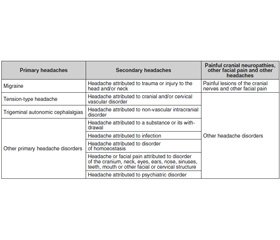
The International Headache Society in 2013 published the international classification of headache disorders, the 3rd edition (Table 1). This document presents diagnostic criteria for the types of primary, secondary headache, cranial neuropathies, primary and secondary facial pain. Secon–dary headaches are considered in terms of acute and chronic headache as a symptom in head and neck injuries, vascular pathology, intracranial non-vascular pathology of the brain, the effects of substances use or their withdrawal, various infections, mental illnesses and other causes [17].
/56-1.jpg)
Differentiation of acute and chronic cephalalgia at infectious diseases is carried out between intracranial (bacterial, viral, fungal meningitis, meningoencephalitis, parasitic infections) and systemic infection. Depending on the stage of the infectious process, the degree and level of damage to the nervous system, the headache associated with infections of different etiologies is often accompanied by fever, nausea/vomiting, meningeal syndrome, rash on the skin of varying severity, asthenic syndrome. More often, a headache is a leading symptom of intracranial infection, while at systemic infections, it is secondary, not prominent. Headache as a cerebral symptom regresses after elimination of viral or bacterial agent. But it can also become a symptom of neuropathic, central pain, becoming chronic during formation of infectious disease consequences, for example, postherpetic neuralgia of the trigeminal nerve.
In the present case, the woman develops secondary recurrent cephalalgia combined with recurrent genital rash of unknown etiology. It should be noted that herpetic etiology of recurrent vesicular exanthema has not been laboratory verified by a reference test based on the analysis of vesicular contents for the presence of HSV 1 + 2 DNA by PCR. However, indirectly, we can suspect HSV infection as the cause of genital rash according to epidemiological data (similar rash was noted in husband), the results of serological tests — the presence of immunoglobulin G to HSV 1 + 2 in the blood, as well as the effectiveness of systemic antiviral chemothera–py with nucleotide analogues, Ac and VAc. Given the long course of the disease, as well as timely link between the onset of genital rash and attacks of cephalalgia, a diagnosis of benign recurrent aseptic meningitis (BRAM) was established. This meningitis is a rare variant of aseptic (lymphocytic) meningitis, having an eponym Mollaret meningitis, named after the French neurologist Pierre Mollaret (1898–1987) [8]. In 1944, in Nazi-occupied France, Pierre Mollaret published in medical journal a clinical observation of three patients, who had recurrent short episodes of headache, fever and vomiting combined with aseptic meningitis, where the so-called phantom cells were present in the CSF, consisting of epithelial cells, lymphocytes and neutrophils [9]. Despite the fact that there were no signs of viral meningitis in the cerebrospinal fluid, which can be explained by the rapidity of CSF normalization in BRAM, which occurs spontaneously within 2 to 5 days (examination of our patient was conducted on day 8 after the onset of the attack), the pre–sence of other signs was consistent with MM criteria (see below) [10–12].
Diagnostic criteria for the diagnosis of Mollaret meningitis (Brynn G.W., 1962) [10]
1. Recurring episodes of severe headache, meningism and fever.
2. Between the attacks, there are normal intervals without any symptoms, lasting from weeks to months.
3. Pleocytosis of cerebrospinal fluid represented by a large number of endothelial cells, neutrophils and lymphocytes.
4. Spontaneous resolution of symptoms.
5. Etiological agent not detected.
Most specialists [13] believe that cases, when the cause of recurrent serous meningitis is not established, are namely MM that is a cross-over, idiopathic version of BRAM. At the same time, as the analysis of the world scientific and medical literature shows, in 84 % of cases, the etiologic factor of BRAM is HSV type 2 [1, 13, 14]. In this regard, it should be noted that the reactivation of HSV type 2 persisting in the sensory ganglia of the lumbosacral spinal cord can also cause combined, but already uroneurological pathology in the form of Elsberg syndrome (Charles Albert Elsberg, 1871–1948), which is manifested as radiculomyelitis (pain/numbness/paresthesia in the buttocks, perineum or legs) in combination with acute urinary retention [12]. Elsberg or MM syndromes demonstrate the pathogenesis of HSV 1 + 2 infection, where infection of sensory ganglia of the autonomic nervous system and lifelong persistence of the virus is a key link explaining the polytopic nature of recurrent pains and somatic pathology. The reasonability of distinction between MM and BRAM is determined by the fact that in the first case, it is necessary to look for causes that are quite extensive (see below) of recurrent inflammation of the soft meninges, while in the second case, it justifies the use of antiherpetic chemotherapy (acyclic nucleotides). At the same time, attention should be paid to the fact that there is no anogenital exanthema at the time of meningitis attack in more than half of the patients [15]. In this regard, administration of acyclic nucleotides in the regime of suppressive chemotherapy in patients with MM is recommended in most guidelines, and under this regime, there is a significant decrease in the incidence of headache and genital exanthema attacks — by 70–80 % [7].
Causes for recurrent benign meningitis [16]
1. Infectious etiological factors:
— viral infections (enterovirus, HSV — Mollaret me–ningitis, HIV, CMV, Epstein-Barr virus, varicella zoster virus, mumps virus):
— bacterial infections (Brucella, Francisella tularen–sis, Actinomyces, Listeria-unpasteurized, Ehrlichia chaf–feensis, Nocardia, rarely — not completely eradicated N.meningi–tidis, Streptococcus or Haemophilus influenzae);
— tuberculous meningitis;
— spirochetoses (Treponema pallidum and Borrelia burgdorferi);
— parameningeal infections;
— fungal infections (Cryptococcus, Coccidioides, Sporothrix, Histoplasma);
— parasitic infections (eosinophilic meningitis — Angio–strongylus, Taenia solium, schistosomiasis, toxoplasmosis).
2. Non-infectious etiological factors:
— tumor;
— sarcoidosis;
— granulomatous angiitis;
— systemic lupus erythematosus and other vasculitis;
— Behcet’s disease;
— Vogt-Koyanagi-Harada syndrome;
— chronic benign lymphocytic meningitis;
— meningitis caused by medication (nonsteroidal anti-inflammatory drugs, trimethoprim/sulfamethoxazole);
— chronic meningitis of unknown etiology.
Practical recommendations
1. Combination of recurrent pain of any localization, such as cephalalgia with neurologic or somatic pathology, includes HSV 1 + 2 infection in the clinical and laboratory differential diagnosis.
2. When establishing the diagnosis of recurrent aseptic meningitis, including MM, etiotropic first line drugs are acyclic nucleotides unless another cause of serous meningitis is found.
3. The acyclovir derivatives in recurrent aseptic me–ningitis, including MM, should be used in the regime of long-term suppressive chemotherapy and should be evaluated exclusively on clinical signs: no relapse of headache, meningitis and anogenital exanthema.
Conflicts of interests. Authors declare no conflicts of interests that might be construed to influence the results or interpretation of their manuscript.
Список литературы
1. Kallio-Laine K., Seppänen M., Kautiainen H. et al. Recurrent lymphocytic meningitis positive for herpes simplex virus type 2 // Emerging Infectious Diseases. 2009; 15(7): 1119-1122.
2. Loren A. Rolak. Neurology Secrets. London (UK): Elsevier Health Sciences, 2008. 584 p.
3. Matthew Robbins, Brian M. Grosberg, Richard Lipton. Hea–dache / John Wiley and Sons Ltd/Wiley-Blackwell. ISBN 978-0-470-65472-9. 2013. 336 p. https://www.bookdepository.com/Headache-Richard-Lipton/9780470654729
4. Diagnosis and management of headache in adults. A national clini–cal guideline. Scottish Intercollegiate Guidelines Network, 2008. 88 p.
5. Steiner T.J., Paemeleire K., Jensen R., Valade D., Savi L., Lainez M.J.A., Diener H.-C., Martelletti P., Couturier E.G.M. European principles of management of common headache disorders in primary care // Journal of Headache and Pain. 2007; 8(1): 57.
6. Joseph R. Berger, Houff S. Neurological Complications of Herpes Simplex Virus Type 2 Infection // Archives of Neurology. 2008; 65 (5): 596-600.
7. David N. Gilbert, Robert C. Moellering Jr., Georg M. Eliopoulos, Henry F. Chambers, Michael S. Saag. The Sanford Guide to Antimicrobial Therapy; Antimicrobial Therapy, Inc., 2016. 688 p.
8. Galdi A.P. Benign recurrent aseptic meningitis (Mollaret’s meningitis) // Arch. Neurol. 1979; 36: 657-658.
9. Mollaret P. Recurrent benign endothelio-leukocytic meningitis. A new syndrome or a new disease? (Case reports) // Rev. Neurol. 1944; 76: 657-658. French
10. Azizul M. Hoque, Chowdhury N., Hoque Z., Siddiqui N. A., Islam R., Ahmad Q. Mollaret’s Meningitis: A Case Report and Review of the Literature // The Journal of Teachers Association. 2004; 17 (1): 41-46.
11. Tedder D.G., Ashely R., Tyler K.L., Levin M.J. Herpes simplex virus infection as a cause of benign recurrent lymphocytic meningitis // Ann. Intern. Med. 1994; 121: 334-339.
12. Katariina Kallio-Laine. Herpes Simplex Virus Infection, Pathological Pain and Recurrent Lymphocytic Meningitis. Helsinki: Academic dissertation, 2009. 83 p.
13. Ahmad K. Abou-Foul, Thajunisha M. Buhary, Sedki L. Gayed. Herpes simplex virus type 2-associated recurrent aseptic (Mollaret’s) meningitis in genitourinary medicine clinic: a case report // International Medical Case Reports Journal. 2014; 7: 31-33.
14. Marwan Shalabi, Richard J. Whitley. Recurrent Benign Lymphocytic Meningitis // Clinical Practice. 2006; 43 (9): 1194-1197.
15. Beloo Mirakhur, Marc McKenna. Recurrent Herpes Simplex Type 2 Virus (Mollaret) Meningitis. Journal of the American Board of Family Medicine. 2004; 17(4): 303-305.
16. Jarrin I., Sellier P., Lopes A. Etiologies and Management of Aseptic Meningitis in Patients Admitted to an Internal Medicine Department // Medicine (Baltimore). 2016; 95(2): e2372.
17. The International Classification of Headache Disorders, 3rd ed. (2013). Headache Classification Committee of the International Headache Society (IHS).

/56-1.jpg)