Международный эндокринологический журнал Том 13, №6, 2017
Вернуться к номеру
Вплив окремих компонентів метаболічного синдрому на функцію нирок при гіпотиреозі (огляд літератури)
Авторы: O.M. Didushko
Higher State Education Institution “Ivano-Frankivsk National Medical University”, Ivano-Frankivsk, Ukraine
Рубрики: Эндокринология
Разделы: Справочник специалиста
Версия для печати
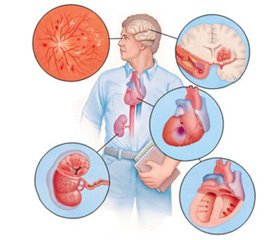
У статті висвітлено вплив окремих компонентів метаболічного синдрому: артеріальної гіпертензії, ожиріння й дисліпідемії на функцію нирок при гіпотиреозі, причинно-наслідковий зв’язок між вказаними компонентами й гіпотиреозом та нирковою дисфункцією. Показано, що артеріальна гіпертензія, абдомінальне ожиріння, гіперлептинемія, дисліпідемія є незалежними факторами ризику розвитку порушення функції нирок при гіпотиреозі.
В статье освещено влияние отдельных компонентов метаболического синдрома: артериальной гипертензии, ожирения и дислипидемии на функцию почек при гипотиреозе, причинно-следственная связь между указанными компонентами и гипотиреозом и почечной дисфункцией. Показано, что артериальная гипертензия, абдоминальное ожирение, гиперлептинемия, дислипидемия являются независимыми факторами риска развития нарушения функции почек при гипотиреозе.
The article deals with the influence of certain components of the metabolic syndrome, such as arterial hypertension, obesity and dyslipidemia, on renal function in hypothyroidism, causal relationship between these components and hypothyroidism and renal dysfunction. It has been shown that arterial hypertension, abdominal obesity, hyperleptinemia and dyslipidemia are independent risk factors for renal dysfunction in hypothyroidism.
гіпотиреоз; артеріальна гіпертензія; ожиріння; лептин; дисліпідемія; хронічна хвороба нирок; огляд
гипотиреоз; артериальная гипертензия; ожирение; лептин; дислипидемия; хроническая болезнь почек; обзор
hypothyroidism; arterial hypertension; obesity; leptin; dyslipidemia; chronic kidney disease; review
- Gerchman F, Tong J, Kristina M, et al. Body mass index is associated with increased creatinine clearance by a mechanism independent of body fat distribution. J Clin Endocrinol Metab. 2009 Oct; 94(10): 3781-8. doi: 10.1210/jc.2008-2508.
- Bonnet F, Marre M, Halimi JM, et al. Waist circumference and the metabolic syndrome predict the development of elevated albuminuria in non-diabetic subjects: the DESIR Study. J Hypertens. 2006 Jun;24(6):1157-63. doi: 10.1097/01.hjh.0000226206.03560.ac.
- Kryachkova AA, Savelyeva SA, Gallyamov MG, Shestakova MV, Kutiryna IM. The role of obesity in renal injury in patients with metabolic syndrome. Nefrologiia i dializ. 2010;12(1):34-8. (in Russian).
- Dobronravov VA, Smirnov AV, Kayukov IG. Manysided albuminuria: aspects of clinical value. Nephrology (Saint-Petersburg). 2009;13(3):33-38. (in Russian).
- Ivanov DD. Lectures on nephrology. Diabetic disease of kidneys. Hypertensive nephropathy. Chronic renal failure. Donetsk: Publisher Zaslavskyi OYu; 2010. 200 p. (in Russian).
- Ivanov DD, Korzh ОM. Nephrology in physician’s practice: study guide. 2nd edition. Donetsk: Publisher Zaslavskyi OYu; 2012. 384 p. (in Ukrainian).
- Damman K, Van Veldhuisen DJ, Navis G, et al. Tubular damage in chronic systolic heart failure is associated with reduced survival independent of glomerular filtration rate. Heart. 2010 Aug;96(16):1297-302. doi: 10.1136/hrt.2010.194878.
- National Kidney Foundation. KDOQI Clinical Practice Guideline for Diabetes and CKD: 2012 Update. Am J Kidney Dis. 2012 Nov;60(5):850-86. doi: 10.1053/j.ajkd.2012.07.005.
- Hojs R, Bevc S, Ekart R, Gorenjak M, Puklavec L. Kidney function estimating equations in patients with chronic kidney disease. Int J Clin Pract. 2011 Apr;65(4):458-64. doi: 10.1111/j.1742-1241.2010.02597.x.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3(1):1–150. doi: 10.1038/kisup.2012.73.
- Waheed S, Matsushita K, Sang Y, et al. Combined association of albuminuria and cystatin C-based estimated GFR with mortality, coronary heart disease, and heart failure outcomes: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Kidney Dis. 2012 Aug; 60(2): 207–216. doi: 10.1053/j.ajkd.2012.03.011.
- Niccoli G, Conte M, Della Bona R. et al. Cystatin C is associated with an increased coronary atherosclerotic burden and a stable plaque phenotype in patients with ischemic heart disease and normal glomerular filtration rate. Atherosclerosis. 2008 Jun;198(2):373-80. doi: 10.1016/j.atherosclerosis.2007.09.022.
- Kravchun NO, Kryvovyaz YuO. Modern diagnostical markers of diabetic nephropathy. Problems of Endocrine Pathology. 2012;3:104-12. (in Ukrainian).
- Shen SJ, Hu ZX, Li QH, et al. Implications of the changes in serum neutrophil gelatinase-associated lipocalin and cystatin C in patients with chronic kidney disease. Nephrology (Carlton). 2014 Mar;19(3):129-35. doi: 10.1111/nep.12203.
- Helal I, Fick-Brosnahan GM, Reed-Gitomer B, Schrier RW. Glomerular hyperfiltration: definitions, mechanisms and clinical implications. Nat Rev Nephrol. 2012 Feb 21;8(5):293-300. doi: 10.1038/nrneph.2012.19.
- Kimmel M, Braun N, Alscher M. Influence of thyroid function on different kidney function tests. Kidney Blood Press Res. 2012;35(1):9-17. doi: 10.1159/000329354.
- Mahmoodi BK, Matsushita K, Woodward M, et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without hypertension: a meta-analysis. Lancet. 2012 Nov 10;380(9854):1649-61. doi: 10.1016/S0140-6736(12)61272-0.
- Zelinska NB. Diagnostics of pathology of cardiovascular system in hypothyroid patients. Clinical Endocrinology and Endocrine Surgery. 2010;1(30):58-60. (in Ukrainian).
- Zubkova SТ. Treatment of primary hypothyroidism: ways to improve. Zdorov’ja Ukrai’ny. 2015;4(32):29-31. (in Russian).
- Mitchenko ОІ, Lohvynenko АО, Romanov VYu. Diurnal profile of blood pressure and structural-functional state of myocardium in patients with metabolic syndrome and thyroid dysfunction, treatment optimization. Ukrainian cardiology journal. 2010;4:70-7. (in Ukrainian).
- Olenych LV, Radchenko ОМ, Bek NS, Olenych LN. The peculiarities of kidney dysfunction in patients with arterial hypertension and obesity under hypothyroidism. Bukovinian Medical Herald. 2015;19(3):118-20. (in Ukrainian).
- Zerbino DD, Bagrij MM, Djadyk OO, et al. Vascular renal pathology: monography. Vinnycja: Nova knyga; 2015. 456 p. (in Ukrainian).
- Butrova SА. Visceral obesity as a key component of metabolic syndrome. Mezhdunarodnyi Endokrinologicheskii Zhurnal. 2009;2(20):82-4. (in Russian).
- Marusyn ОV, Bociurko VІ. Obesity and leptin resistance. Galician medical journal. 2012;19(1):155-7. (in Ukrainian).
- Pertseva ТА, Rokutova MK. Obesity and metabolic syndrome: relation to renal dysfunction. Urology. 2010;1:52-8. (in Russian).
- Kryachkova AA, Savelyeva SA, Gallyamov MG, Shestakova MV, Kutiryna IM. The role of obesity in renal injury in patients with metabolic syndrome. Nefrologiia i dializ. 2010;12(1):34-8. (in Russian).
- Kutyrina IМ, Krуachkova АА, Savielieva SА. The role of hyperinsulinemia and insulin resistance in development of chronic kidney disease in patients with metabolic syndrome. Terapevticheskij arkhiv. 2012;84(6):32-6. (in Russian).
- Pertseva TO, Rokutova MK. Influence of insulin resistance on renal function in patients with abdominal obesity. Medicni perspektivi. 2015;20(2):30-6. (in Ukrainian).
- Pertseva TO, Rokutova MK, Tadgieva EI. The influence of cardiovascular risk factors on glomerular filtration rate in young patients with abdominal obesity. Urology. 2012;16(3(62)):38-44. (in Ukrainian).
- Saginova EA, Gallyamov MG, Severova MM, et al. The role of leptin, adiponectin and insulin-resistance markers in development of early stages of chronic kidney disease and atherosclerosis of carotid arteries in obese patients. Terapevticheskij arkhiv. 2011;83(6):47-53. (in Russian).
- Fedorova EU, Kutyrina IM. Mechanisms of progression of kidney injury in obesity. Nefrologiia i dializ. 2006;8(2):102-11. (in Russian).
- Petunina NА, Al`tshuler NE, Rakova NH, Trukhina LV. Hormones of the adipose tissue and functional activity of the thyroid. Obesity and metabolism. 2010;7(4):8-11. (in Russian).
- Zakharova SМ, Savielieva LV, Fadeeva MI. Obesity and hypothyroidism. Obesity and metabolism. 2013;2(35):54-8. (in Russian).
- Baig M, Azhar A, Zaidi P, Kamal S, Karira K. Serum leptin level in hypothyroid males. J Coll Physicians Surg Pak. 2005;15(12):757-60. doi: 12.2005/JCPSP.757760.
- Nyrnes A, Jorde R, Sundsfjord J. Serum TSH is positively associated with BMI. Int J Obes (Lond). 2006 Jan;30(1):100-5. doi: 10.1038/sj.ijo.0803112.
- Papafragkaki DK, Tolis G. Obesity and renal disease: A possible role of leptin. Hormones (Athens). 2005 Apr-Jun;4(2):90-5. PMID: 16613810.
- Korpachev VV, Kushnar’ova NM. Features of fatty-acid spectrum of triglycerides in patients with insulin resistance and metabolic syndrome. Lik Sprava. 2009 Oct-Dec;(7-8):50-5.
- Mitchenko OI, Logvinenko AO, Romanov VYu. Diurnal profile of blood pressure and structural-functional state of myocardium in patients with metabolic syndrome and thyroid dysfunction, treatment optimization. Ukrainian cardiology journal. 2010;4:70-7. (in Ukrainian).
- Pan’kiv VІ. Practical thyroidology. Donetsk.: Publisher Zaslavskyi OYu; 2011. 224 p. (in Ukrainian).
- Mitchenko ОІ, Lutaj МІ. Dyslipidemia: diagnosis, prevention and treatment. Kyi’v: Chetverta hvylja; 2007. 56 p. (in Ukrainian).
- Mitchenko ОІ, Lohvinenko АО, Romanov VYu. The optimisation of lipid and carbohydrate exchange correction in patients with metabolic syndrome and thyroid dysfunction. Ukrainian cardiology journal. 2010;1:73-80. (in Ukrainian).
- Kolina IB. Hyperlipidemia in chronic kidney disease: peculiarities and approaches to treatment. Lechashchii vrach. 2012;1:63-70. (in Russian).
- Loboda OM, Dudar IO. Dislipidemia in patients with chronic kidney disease. Ukrainian journal of nephrology and dialysis. 2014;2:50-61. (in Ukrainian).
- Calabia J, Torguet P, Garcia I. et al. The relationship between renal resistive index, arterial stiffness, and atherosclerotic burden: the link between macrocirculation and microcirculation. J Clin Hypertens (Greenwich). 2014 Mar;16(3):186-91. doi: 10.1111/jch.12248. Epub 2014 Feb 19.